Da Vinci Payer Data Exchange, published by HL7 International / Financial Management. This guide is not an authorized publication; it is the continuous build for version 2.1.1 built by the FHIR (HL7® FHIR® Standard) CI Build. This version is based on the current content of https://github.com/HL7/davinci-epdx/ and changes regularly. See the Directory of published versions
| Page standards status: Informative |
Previous Page - Security and Privacy
This section defines the Actors, Exchange Interactions and Data Payloads covered by the PDex IG.
The Member Health History is represented as a series of FHIR Resources that are based on a superset of US Core 3.1.1 or US Core 6.1.0, HRex and PDex profiles. The content/payload of the Member Health History may be augmented by FHIR resources that are generated from other HL7 Da Vinci IG use cases, such as Coverage Requirements Determination(CRD) or Prior Authorization Support (PAS).
The following actors are recognized in the PDex IG:
There are different terms used for an individual or patient in the Health Plan industry. Terms such as subscriber or member may be used. A subscriber and a member are not necessarily equivalent. For example, the subscriber may be the primary family member on a plan that covers the entire family. Therefore, the term Member will be used throughout this guide to identify the individual subject of the "member health history".
The PDex IG is specifying three exchange interactions:
The PDex IG defines two types of data payload:
All resources and operations available via a FHIR API endpoint SHALL be declared in a FHIR CapabilityStatement. §pdex-198
See Data Mapping for details of the Data Payloads and operations.
The PDex IG is focused on provider, member, or plan directed exchange of a member's data.
All exchanges in this IG are for an individual. Where one member has permission to access the information for another member of the health plan, they SHOULD provide appropriate credentials to enable the exchange for that individual.
The PDex IG specifies three interaction methods. Their use depends upon the Actors involved and the Data Payloads being exchanged.
There are three potential interaction methods:
This version of the IG adds new APIs that support the requirements of the CMS Prior Authorization Rule (CMS-0057). These APIs are:
Earlier versions of the PDex IG recommended the use of CDS Hooks to enable Provider Access to ember data. That method has been superceded by the Provider Access API that meets the requirements of the CMS Prior Authorization Rule (CMS-0057).
Note: This section is being considered for removal in the next release of this IG.
Clinical systems will use the specification and workflows defined by CDS Hooks to initiate Payer Data Exchange with Health Plans. Implementers must be familiar with all aspects of this specification.
SMART-on-FHIR is expected to be used in conjunction with CDS Hooks in two principal ways:
The CDS Hooks and SMART-on-FHIR application configuration is detailed in CDS-Hooks.
The specification of a SMART-on-FHIR App to initiate a CDS-Hook call to a Health Plan's FHIR API enables:
CDS Hooks provides a mechanism for providers/clinicians to request a medical history for their patient from the Health Plan as part of their regular workflow - when scheduling an appointment. However, sometimes clinicians may be interested in updating the patient's medical history without going through the appointment booking steps within their EMR. I.e., They don't want to actually create an appointment, they just want to ask the question "Has anything new happened to my patient at some other location?"
Sometimes clinicians want to check and update a patient's history, for example during a patient review, or responding to a question from a patient. One solution to this need is the use of a SMART on FHIR app that will invoke a CDS Hook. This is possible because many EMR systems provide support for SMART on FHIR. This use of SMART is distinct from the use of SMART in CDS Hooks. This isn't launching a SMART app based upon the contents of a returned card. Instead, it is using SMART to invoke a CDS Hook in place of the EMR. It is emulating the workflow trigger that would normally trigger a hook within an EMR workflow.
The SMART on FHIR CDS Hook trigger approach was pioneered by the Da Vinci Coverage Requirements Discovery IG (CRD-IG). Developers interested in using this approach should refer to the CDS Hooks and SMART on FHIR sections of that IG for the latest guidance, examples and links to code samples.
The PDex IG uses a similar approach to enable a CDS Hook. The CDS Hook used by PDex is:
This IG also proposes the creation of a new CDS Hook for the interaction defined in this IG. This hook would be:
An overview of the transaction flow is shown in figure 4-1:
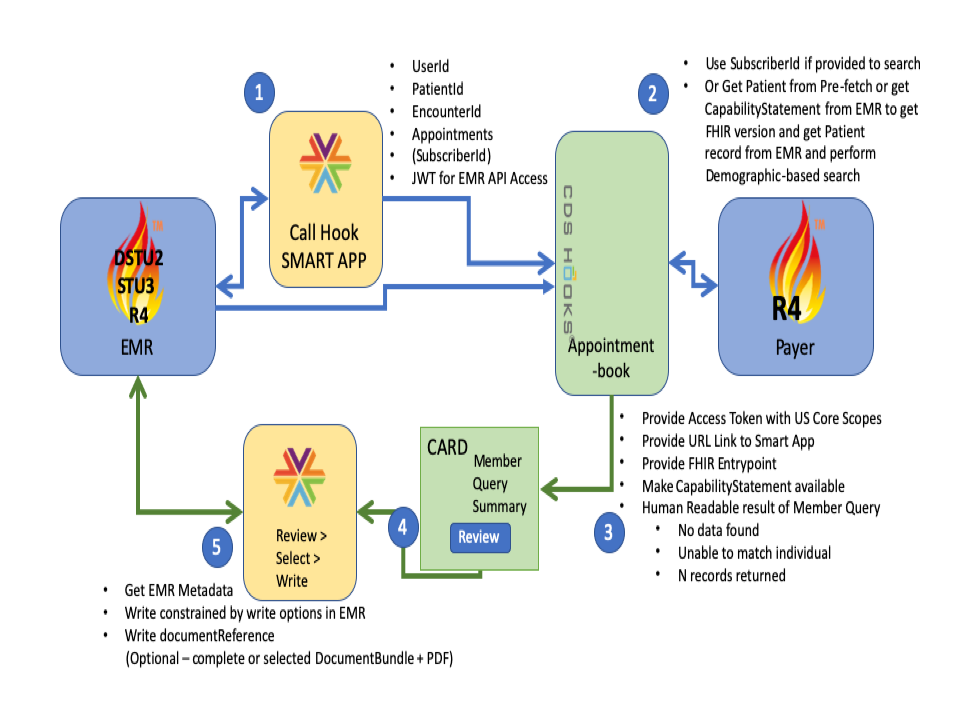 **Figure 4-1: CDS-Hooks SMART-on-FHIR Transaction Flow
**Figure 4-1: CDS-Hooks SMART-on-FHIR Transaction Flow
When a Health Plan server responds to a CDS Hook, one of the possible actions is to allow the user to invoke a SMART App. Support for this option by Health Plan systems SHOULD be provided. §pdex-199 The SMART on FHIR app provided as a link from the returned CDS Hook SHOULD enable a clinician to §pdex-200 review the available Health Plan's data for their patient, select the data they want to commit to their EMR system and upon confirming their selection, enable the selected data to be written to the clinician's EMR system.
The objective of this flow is to place the decision about the data being deposited into the EMR into the hands of the responsible organization and their providers. This does not prevent an organization from defining data selection criteria that filters Health Plan provided information and automatically importing records that meet their criteria. For the purposes of this IG and accompanying Reference Implementation the manual provider selection method was used to illustrate the record import capability.
The Da Vinci Documentation Templates and Rules Implementation Guide (DTR-IG) provides additional guidance and expectations on the use of CDS Hook cards to launch SMART Apps and how payer-provided SMART Apps should function.
All requesters (e.g., EHRs) SHOULD store provenance associated with any data exchanged as part of this IG if §pdex-201 it is committed to their system.
This section outlines the approach for a member to mediate the sharing of data between health plans, or with an app of their choice using the Patient Access API and the SMART-on-FHIR App Launch methods. If a Payer, as the new health plan, wished to offer members the ability to retrieve data from prior health plans they would need to provide an application that could be registered with other health plans to enable members to authenticate with their prior health plan and authorize sharing with their new health plan. The application would then retrieve data that is shared via the Patient Access API and could load that data into the member's record.
In the STU 2.1 version of the Payer Data Exchange (PDex) IG additional bulk exchange methods are defined that enable data exchange to occur between health plans (Payer-to-Payer Bulk Exchange), at the direction of the member, or to enable exchange with a Provider (Provider Access API) unless a member has actively opted-out of data sharing with Providers.
The well-defined mechanism for enabling Member/Patient authorization to share information with an application using the FHIR API is to use OAuth2.0 as the Authorization protocol. The member SHALL authenticate using §pdex-202 credentials they have been issued by the Health Plan. This is typically the member's customer portal credentials.
The member will typically select a third-party application, service or new (target) Health Plan with whom they wish to share data. The member should review and agree with the Terms of Service and a Privacy Policy that details how the application or service will use the member's data from the (source) Health Plan. While authenticated to the application or service, the member MAY connect to the (source) Health Plan's §pdex-203 authorization server. After authenticating to the (source) Health Plan's authorization server, the Member SHALL be presented with an Authorization screen that enables them to approve the sharing of information with §pdex-204 their intended application, service or (target) Health Plan. For this authorization to occur the Application, service or (target) Health Plan will require OAuth 2.0 client application credentials that are issued by the (source) Health Plan in order to register an authorization request.
The Authorization process, in accordance with applicable privacy policy, SHALL provide a mechanism to §pdex-205
support current regulations allowing members the right to decide what information is permitted to be exchanged.
Examples of member authorized restrictions/permissions are 42CFR, State and Federal requirements for sensitive data.
After successfully authorizing an application an Access Token and Optional Refresh Token SHALL be §pdex-206 returned to the requesting application.
The scopes of the access token SHALL be restricted to the authorizing Member's information and the scopes approved. §pdex-207
Any subsequent Access Token issued based on the Refresh Token SHALL be restricted (at least) to the same §pdex-208 restrictions.
The requesting application SHALL use the access token to access the Health Plan's secure FHIR API to download §pdex-209 the information that the Application is allowed to access.
The OAuth2.0 Member-authorized exchange is detailed in Section: Member-Authorized OAuth2.0 Exchange.
An overview of the OAuth2.0 Flow using the FHIR API is shown below for both Health Plan exchange and Third-Party Application Exchange:
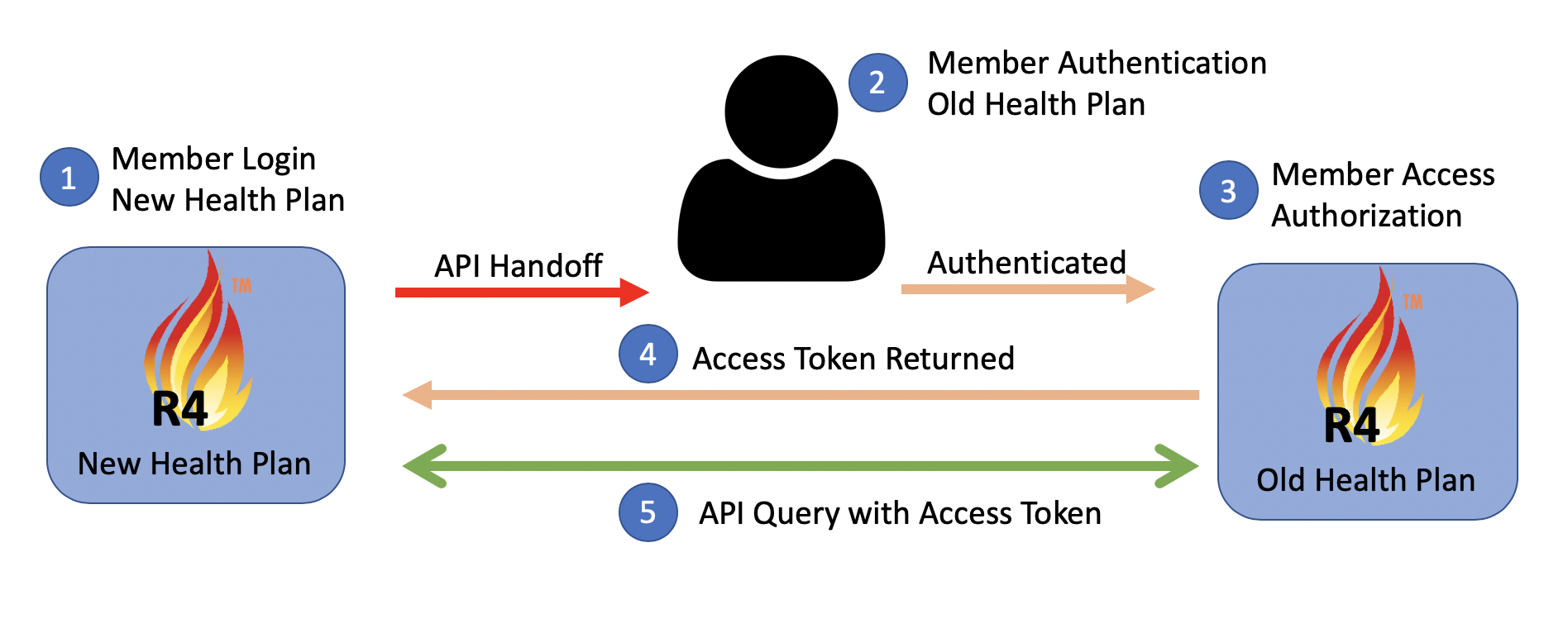 **Figure 4-2: Payer-to-Payer Exchange with Member Interaction
**Figure 4-2: Payer-to-Payer Exchange with Member Interaction
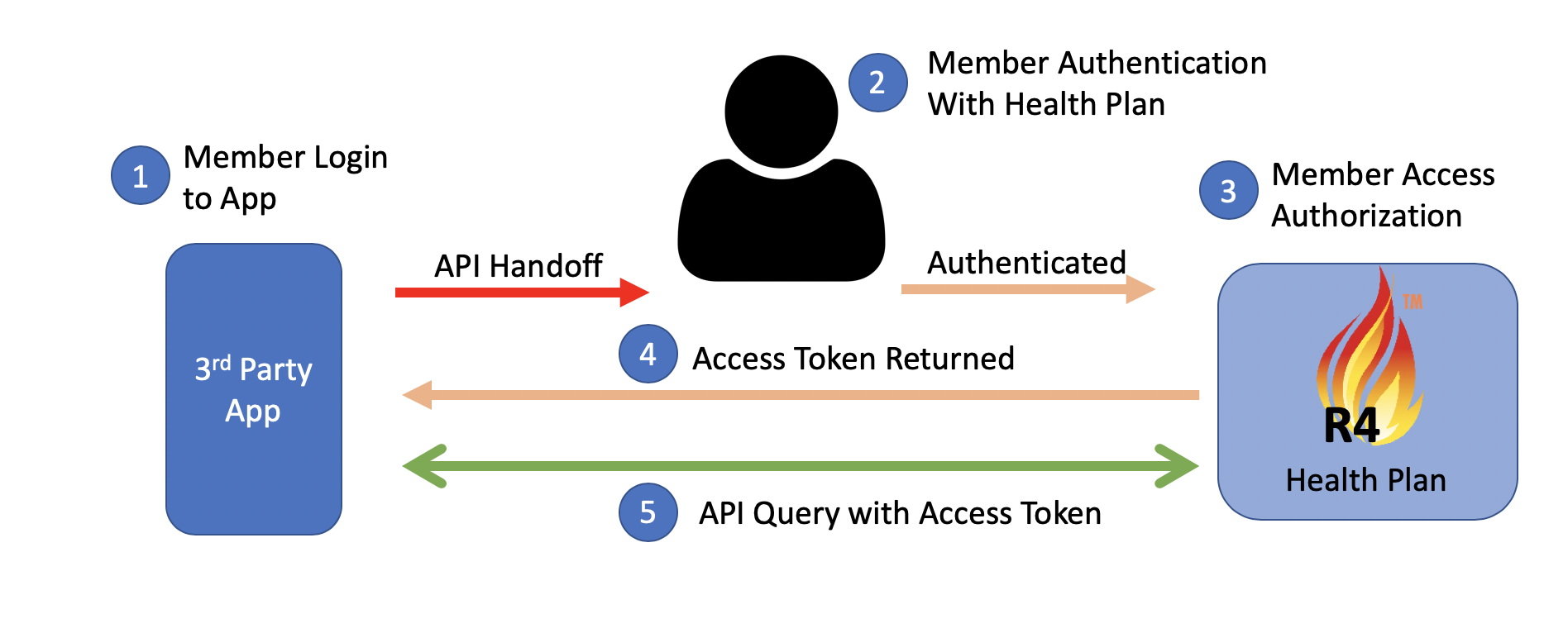 **Figure 4-3: Payer to Application Interaction
**Figure 4-3: Payer to Application Interaction
The Exchange of all of a member's clinical data, as scoped by USCDI version 1 or version 3 and represented in FHIR by US Core 3.1.1 or US Core 6.1.0, is a requirement of the CMS Prior Authorization Rule (CMS-0057).
The CMS Prior Authorization Rule (CMS-0057) requires Payers to make available Prior Authorization decisions and updates via the Patient, Provider and Payer-to-Payer Access APIs. The Rule also requires the exchange of the supporting clinical data, used in arriving at the Prior Authorization decision, (based on US Core 3.1.1 and, in the future, US Core 6.1.0) via those same APIs.
For Patient and Provider Access APIs, the requirement is to exchange structured clinical data used in arriving at the Prior Authorization Decision.
For the Payer-to-Payer API, the rule also requires any Unstructured data used in arriving at the Prior Authorization decision to be exchanged.
Payer-to-Payer exchange can be accomplished by two methods:
Clients wishing to retrieve data SHOULD consult the Data Provider's Server Capability Statement to §pdex-210 determine which methods are made available by the data holder.
The exchange of Unstructured data does not require a Payer to translate the unstructured content into structured FHIR resources such as Observations or Conditions, etc.
Payers SHOULD: §pdex-211
Payers are required to exchange Unstructured data with other Payers via the Payer-to-Payer API.
Payers MAY choose to exchange unstructured data with Patients and Providers, via their respective APIs, §pdex-212 using the same content provided to Payers. i,e. Attaching as a binary resource and referenced in a DocumentReference.