Da Vinci Payer Data Exchange, published by HL7 International / Financial Management. This guide is not an authorized publication; it is the continuous build for version 2.1.1 built by the FHIR (HL7® FHIR® Standard) CI Build. This version is based on the current content of https://github.com/HL7/davinci-epdx/ and changes regularly. See the Directory of published versions
| Page standards status: Informative |
Previous Page - Workflow Examples
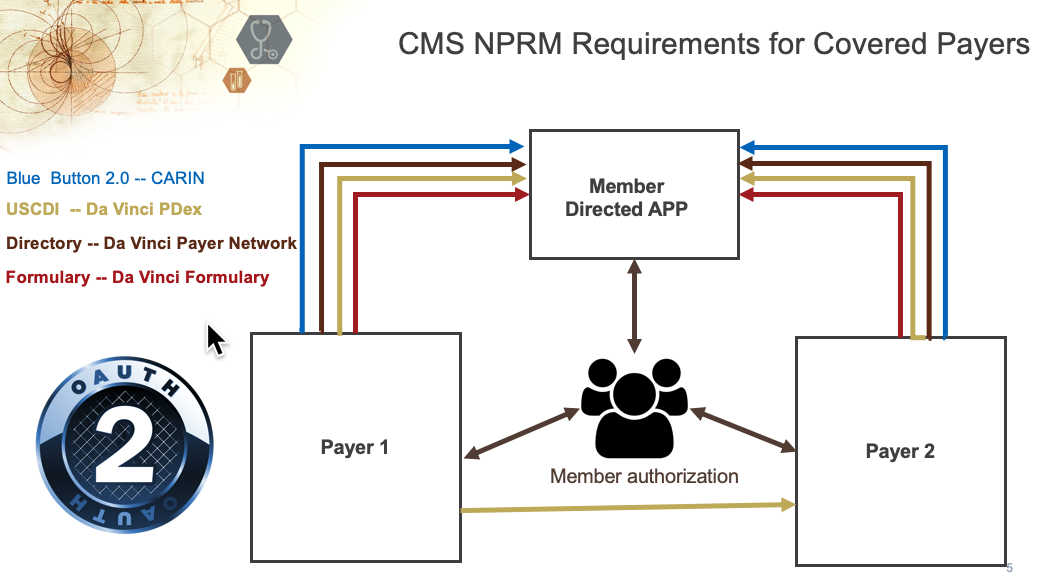
This IG provides a mechanism for Member-authorized exchange of their Health History:
The authorization method uses the OAuth 2.0 protocol to issue a token to an authorized application or service. The authorized application can then use the token to enable interaction with the FHIR REST API.
When a Member is authorizing sharing of the Member Health History with another Health Plan, or a Third Party Application, via the OAuth 2.0 protocol the Health Plan that is operating the API SHALL offer the Member an option to allow the sharing of sensitive information, such as behavioral health data, resulting in the data being shared excluding sensitive data that is covered by state and/or federal regulations. §pdex-104 However, under the HIPAA Right of Access the Member is at liberty to share that information if they so wish.
|
The well-defined mechanism for enabling Member/Patient authorization to share information with an application using the FHIR API is to use OAuth2.0 as the Authorization protocol. The member SHALL authenticate using credentials they have been issued by, or accepted by the Health Plan. §pdex-105 This is typically the member's customer portal credentials.
After authenticating the Member SHALL be presented with an Authorization process that enables them to approve the sharing of information with the Third Party, or new Health Plan, Application that has client application credentials registered with the Health Plan. §pdex-106
The Authorization process SHALL provide the ability for the authorized representative to designate a third-party application that will have access to all information permitted by current state and federal regulations. §pdex-107
After successfully authorizing an application an Access Token and Optional Refresh Token SHALL be returned to the requesting application. §pdex-108
The requesting application SHALL use the access token to access the Health Plan's secure FHIR API to download the information that the Member is allowed to access. §pdex-109
Applications are registered with the API Endpoint. The application owner MAY be: §pdex-110