Standardized Medication Profile (SMP) FHIR IG, published by HL7 International / Pharmacy. This guide is not an authorized publication; it is the continuous build for version 1.0.0 built by the FHIR (HL7® FHIR® Standard) CI Build. This version is based on the current content of https://github.com/HL7/smp-ig/ and changes regularly. See the Directory of published versions
| Page standards status: Informative |
This section of the implementation guide defines the specific requirements for systems wishing to conform to Standardized Medication Profile implementation guide. The Representational State Transfer (REST)-based exchanges of resources is the primary means of information exchange. In some cases, it is more efficient to submit a FHIR Bundle that includes the primary Medication List resources along with all referenced SMP Medication Statements, consolidating the exchange into a single REST request.
Before reading this formal specification, implementers should first familiarize themselves with two other key portions of the specification:
The Use Cases & Overview page provides context for what this formal specification is trying to accomplish and will give a sense of both the business context and general process flow enabled by the formal specification below.
The Technical Background page provides information about the underlying specifications and indicates what portions of them should be read and understood to have the necessary foundation to understand the constraints and usage guidance described here.
This implementation guide uses specific terminology to flag statements that have relevance for the evaluation of conformance with the guide:
SHALL indicates requirements that must be met to be conformant with the specification.
SHOULD indicates behaviors that are strongly recommended (and which may result in interoperability issues or sub-optimal behavior if not adhered to), but which do not, for this version of the specification, affect the determination of specification conformance.
MAY describes optional behaviors that are free to consider but where there is no recommendation for or against adoption.
This implementation guide sets expectations for both clients and servers during the transition of care and the exchange of Standardized Medication Profiles. In a transition of care, one FHIR Server for an organization may act as a client to a FHIR Server for a second organization (with additional system configurations and intermediaries possible). For the use case where the organization responsible for patient following the transition is known, the pre-transition organization may push information to the destination. In all cases, the pre-transition organization must be able to support queries for previous medication lists.
This specification makes significant use of FHIR profiles and terminology artifacts to describe the content to be shared as part of transition of care process.
The full set of profiles defined in this implementation guide can be found by following the links on the Artifacts page.
The primary interaction supported by this implementation guide is POST and GET. As an alternative to the granular REST transactions there are optional operations defined.
The interactions can be comprised of completely RESTful operations for the storage and retrieval of resources but there are situations where the submission of a transaction Bundle containing the primary List resource and all of the associated MedicationStatement resources would be appropriate. As an alternative, where allowed by the server, use the Bundle Medication List and Bundle Medication List Maintenance profiles and the SMP Operation Retrieve and SMP Operation Submit operations.
When using a Bundle, the first entry in the Bundle SHALL be a List resource complying with the MedicationList defined in this IG to ensure the content is sufficient to appropriately populate a full medication list.
All resources SHALL comply with their respective profiles. FHIR elements not marked as 'must support' MAY be included in resources, but client systems should have no expectation of such elements being processed.
All transactions in SMP are synchronous and SHALL require one of the following HTTP responses:
If an OperationOutcome is received, it may have information regarding errors that should be addressed in the future, but did not cause the transaction to fail. NOTE: These errors should not be returned to the provider but should be reviewed and addressed by technical staff.
| Element | Cardinality | Datatype | Information |
|---|---|---|---|
| Severity | 1..1 | code | fatal, error, warning, information |
| Code | 1..1 | code | IssueType |
| Details | 0..1 | CodeableConcept | additional code that clarifies the issue type |
| Diagnostics | 0..1 | string | addl information (response from validation, TA1, 999) |
| Expression | 0..* | string | FHIRPath of element(s) |
Using the base use case scenarios, the following diagrams show the information flows across multiple transitions of care and the use of the SMP profiles to support and enhance the information exchange
The abbreviations that appear in the following workflows are defined as:
| Abbrev. | Expansion |
|---|---|
| EHR | Electronic Health record system |
| HDM | Health Data Manager - a generalized term for a centralized repository or exchange to help locate and retrieve patient's records. This may be a central repository within a health system or a mechanism to allow retrieval from a group of federated repositories. |
| HHA | Home Health Authority |
| SNF | Skilled Nursing Facility |
All of the information exchanges described in the following sections cover the transitions between care facilities and do not cover the internal events that will update and alter the medication lists during a patient's inpatient stay.
In the interaction diagrams following, the Bundle versions of the updates and retrievals have been used to simplify the diagrams. It is possible to store and retrieve individual resources and still meet the use case requirements with additional interactions between servers and clients.
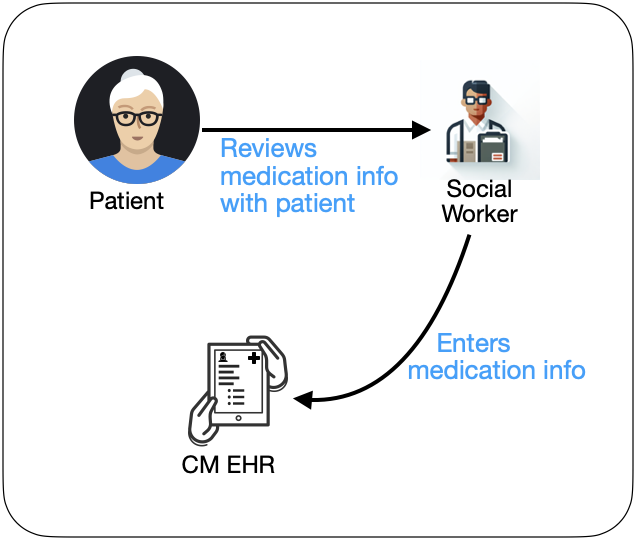
In the initial diagram the capture of the patient medications, including both prescription and non-prescription items is performed and the information is record via a List resource and MedicationStatement resources as needed.
See abbreviations above for a description of Health Data Manager
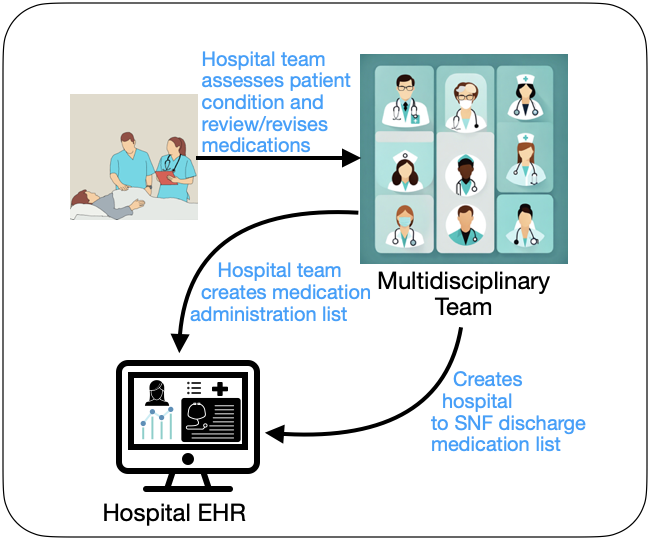
Following the stroke event the patient is admitted to hospital, previous medications (via the list created in A.1) are reviewed and based on treatment, the hospital administration list is created. When the patient is stabilized and ready for discharge to the rehabilitation facility, the discharge list is created.
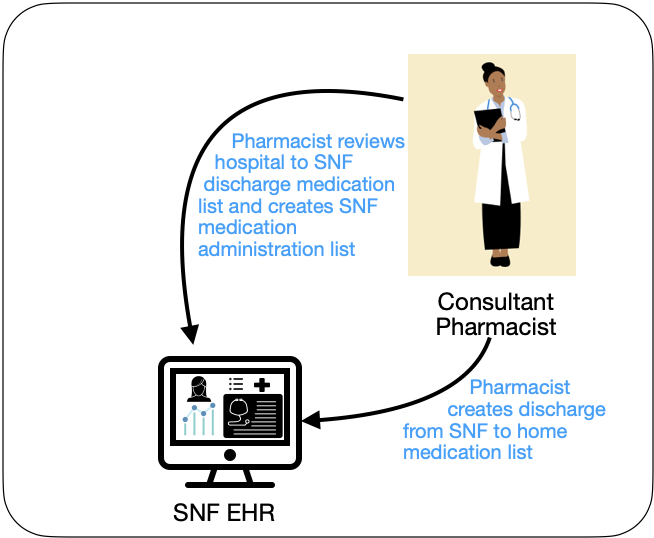
The hospital discharge list is reviewed and revised to create the administration list for the Skilled Nursing facility (SNF). This list is updated during the patients stay in the facility. As medications are removed from the administration list, they are added to the discontinued medication list.
When rehabilitation in the SNF is complete the patient is ready to be returned to the home setting. Here the care team at the SNF prepare the SNF Discharge Medication list.
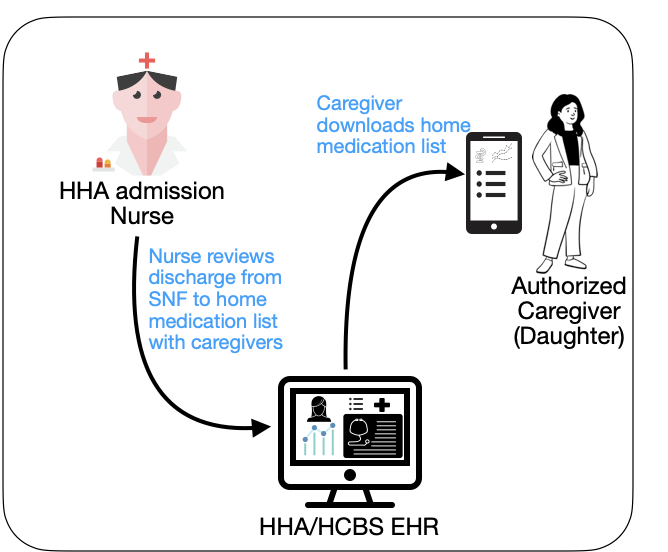
Back in the community, the home care team for the patient review the discharge medication list from the SNF (and may also review previous administration lists and the discontinued medication list), making any recommendations as appropriate and create the new home medication list.
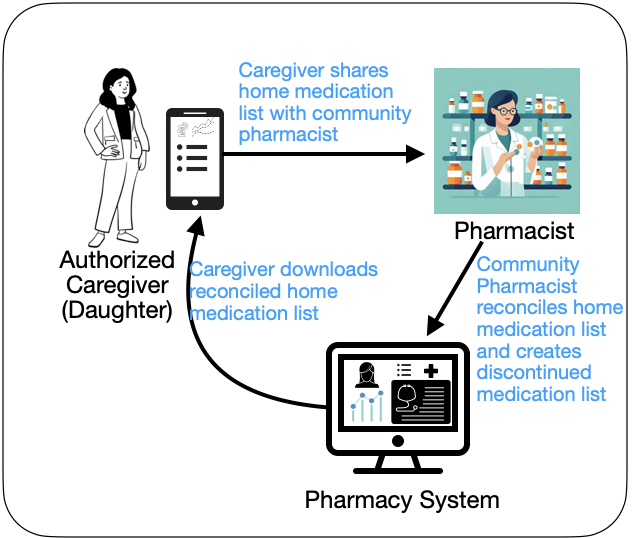
The Primary caregivers go to the community pharmacy, the home care team for the patient review the discharge medication list from the SNF (and may also review previous administration lists and the discontinued medication list), making any recommendations as appropriate and create the new home medication list. The community pharmacist provides the medications to the caregiver with instructions, the caregiver can also access the current home medication list from the patient portal of the Home Health Authority system.
The diagram below illustrates the structure of the relationships between the various resources in this IG. The resources present the internals as accurately as possible with some shortcuts to flatten the JSON structure (collapsing arrays to a single indexed attribute '[0]' for example or collapsing structure to a single attribute 'dosage.text'). Because of these simplifications and the use of placeholders, the depicted resources are illustrative and may not be fully valid FHIR instances. They are intended to show where data is represented and how resources reference each other across the overall resource graph. The Patient resource instance is only provided once on the diagram, the additional references to the Patient resource instance all use the 'Patient/identifier' and appear in red text and underlined.
The diagram has been constrained to common browser widths. Open the diagram in its own window to view full-size.
It is the intent of this implementation guide to provide specifications for the exchange of medication information in a way that is conducive to developing test scripts and a reference implementation (RI) that can be used to validate/exercise the IG at connectathons and during piloting and production deployment. It is also the intent of this guide that any test scripts will include testing of: