Potential Drug-Drug Interaction (PDDI) CDS IG : STU1 Ballot 2, published by HL7 Clinical Decision Support Workgroup. This guide is not an authorized publication; it is the continuous build for version 1.0.0-ballot built by the FHIR (HL7® FHIR® Standard) CI Build. This version is based on the current content of https://github.com/HL7/PDDI-CDS/ and changes regularly. See the Directory of published versions
PDDI CDS knowledge artifacts.
CDS Hooks.
order-select service (if used) SHOULD include medication resources but could include Condition or other resources important for the service to assess for PDDIsA CDS rule execution engine (service).
The CDS rule execution engine SHOULD be able to process CDS Hooks requests and return CDS Hooks Card responses. In processing a CDS request, it SHOULD also be able to process FHIR data including clinical and terminology resources.
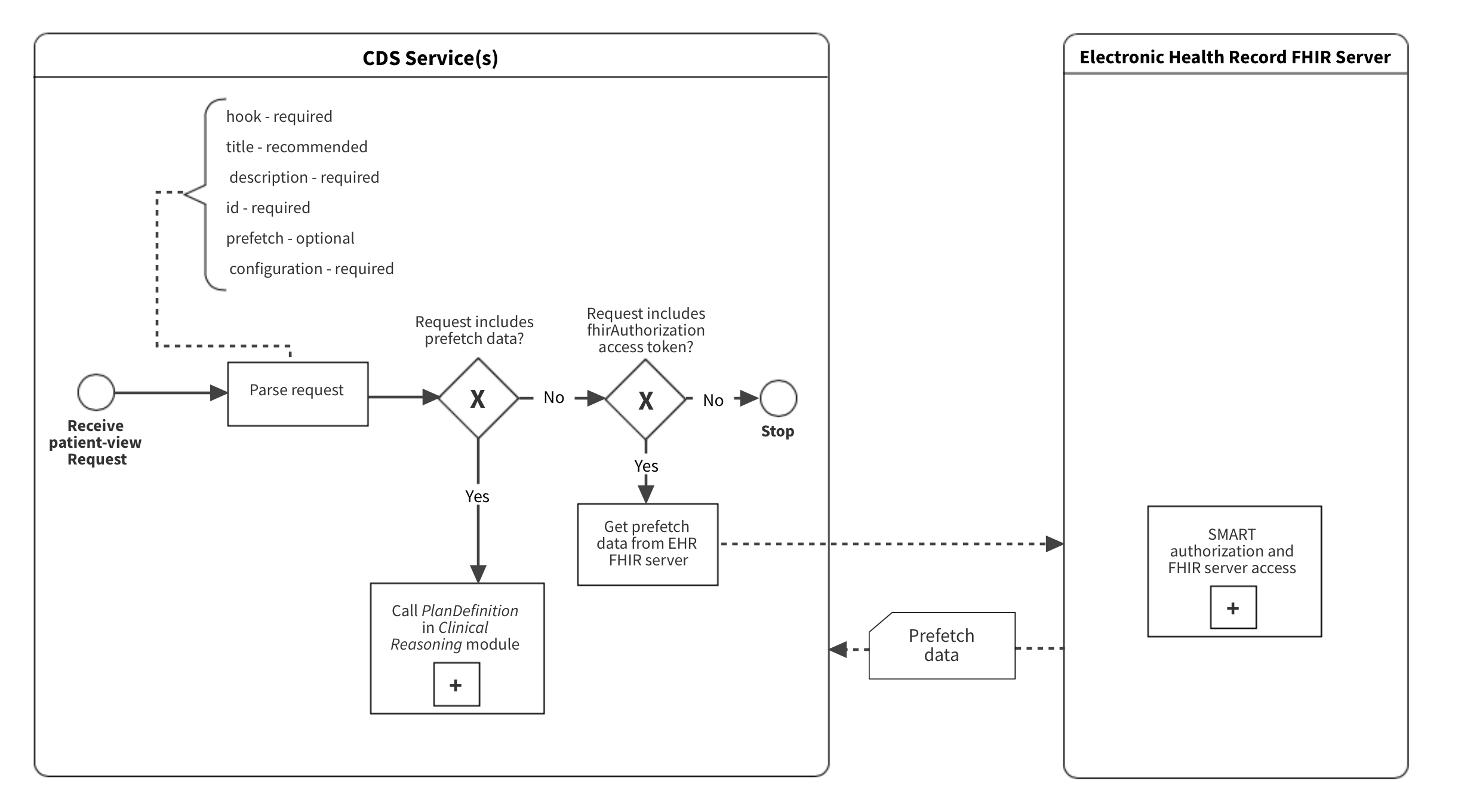
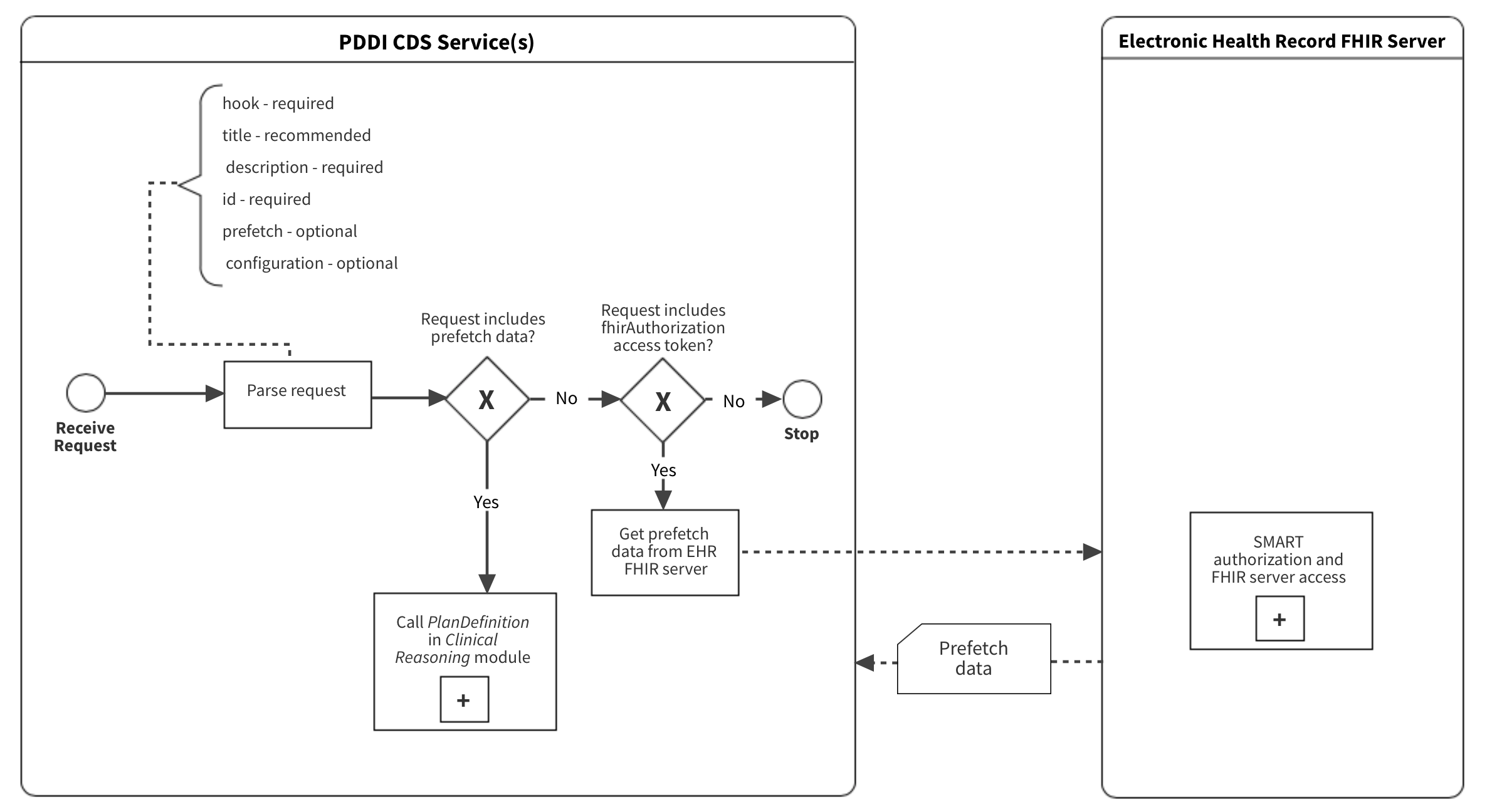
If the CDS rule execution engine does not receive prefetch data in the request it SHOULD query the FHIR server via network call.
A rule engine MAY execute CDS rules written in CQL and represented as a FHIR Library, either directly or compiled to Expression Logical Model. While this method is described in the current IG, implementers MAY choose to use various programming languages, rule engines and/or machine learning models rather than CQL+FHIR.
If the engine implements the advanced functionality described in this implementation guide (i.e., coordination between order-select and order-sign to prevent alert duplication) then, it SHOULD support processing of the configuration options described in Extension subsection. If EHR clients do not send the configuration options, the default behavior of the service should be to NOT suppress card responses at order-sign that might duplicate card responses sent at order-select. This is because the EHR client should have an active role in the decision of whether to filter out alert responses.
It is RECOMMENDED that the rule engine not be given permission to access information that is masked from the clinician whose EHR session has triggered the CDS request (aka 'super user' status) unless there is a specific Break the Glass (BTG) procedure that covers such situations. If there a valid BTG procedure that allows the rule engine to access such information, it SHOULD return an information card stating that such a directive is present. The CDS card SHOULD include that the clinician will be held accountable for BTG throughout any related system audit.
A CDS service MAY choose to use a DetectedIssue resource to convey additional information about a drug-drug interaction. If a DetectedIssue is provided, it SHOULD be incorporated within the CDS Hooks response as a suggested action with type create.
An electronic health record (EHR) CDS client.
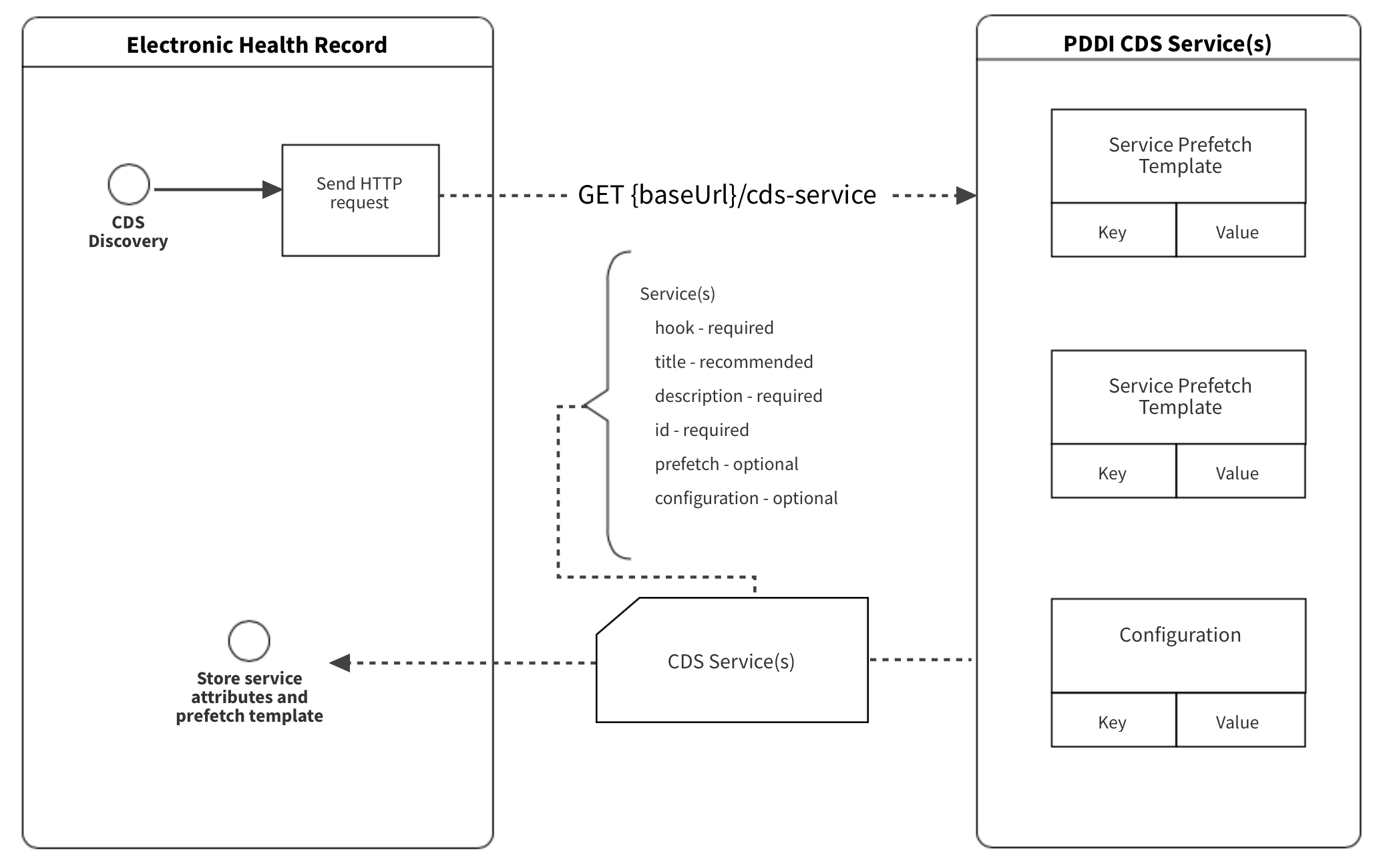
Prior to a hook trigger and subsequent processes, the EHR SHOULD initiate a CDS Discovery request. The CDS discovery response is for the system and would not be viewed by the clinician.
The EHR SHOULD call the PDDI CDS service by sending an HTTP POST containing a CDS Hooks request (JSON formatted) to the service endpoint (e.g.,http://FHIR.org/PDDI-CDS/warfarin-nsaids-cds). The JSON (CDS Hooks request) SHOULD contain specified information for the hook that was triggered including FHIR server, user, and context. Provision of prefetch data as specified by the CDS service is RECOMMENDED.
If the EHR client is requesting a CDS from an engine implements the advanced functionality described in this implementation guide (i.e., coordination between order-select and order-sign to prevent alert duplication) then, the client SHOULD use the configuration options described in Extension subsection. The purpose of this is so that the EHR client has an active role in the decision to filter out alert responses.
This section contains documentation on how to implement PDDI CDS artifacts from a clinical and technical perspective. Later sections describe implementation details using a specific knowledge artifact example. Structured artifacts that implement the logic and behavior described below are available under Artifacts.
The words SHOULD, SHOULD NOT, REQUIRED, SHALL, SHALL NOT, SHOULD, SHOULD NOT, RECOMMENDED, MAY, AND OPTIONAL are used as defined "Key words for use in Request for Comment (RFC) to Indicate Requirement Levels". S. Bradner. IETF. March 1997. Best Current Practice.
A web service that processes CDS requests using a CDS rule execution engine. The service SHOULD be able to process CDS Hooks requests and return CDS Hooks Card responses.
A web service that processes CDS requests SHOULD be able to process FHIR data including clinical and terminology resources.
The EHR system that sends requests to the service MAY provide access to the service to relevant patient data in the EHR via a FHIR server. EHR systems that do not provide access to addition patient data will potentially receive more limited CDS because the service will only work with data in the context and prefetch fields of CDS Hooks requests.
To invoke the PDDI CDS service, the EHR needs to send a CDS Hooks request at a pre-specified step the workflow process. The CDS service then parses and processes the request to determine if the prescribed medication conflicts with a medication the patient is presumably taking. If this condition is satisfied, the CDS service provides individualized information based on the PDDI knowledge base. While each implementation may employ a slightly different approach to ensure successful integration of the CDS system. Here are several general aspects to assess:
A technical framework for the EHR to interact with the CDS service by
creating and sending CDS Hooks requests
capturing and presenting CDS Hooks card responses
Use of FHIR terminologies (e.g., RxNorm, LOINC) and other FHIR resources
SMART authentication during FHIR server requests
NEED TO ADD SECTION REGARDING EVIDENCE RESOURCE AND EBM ON FHIR
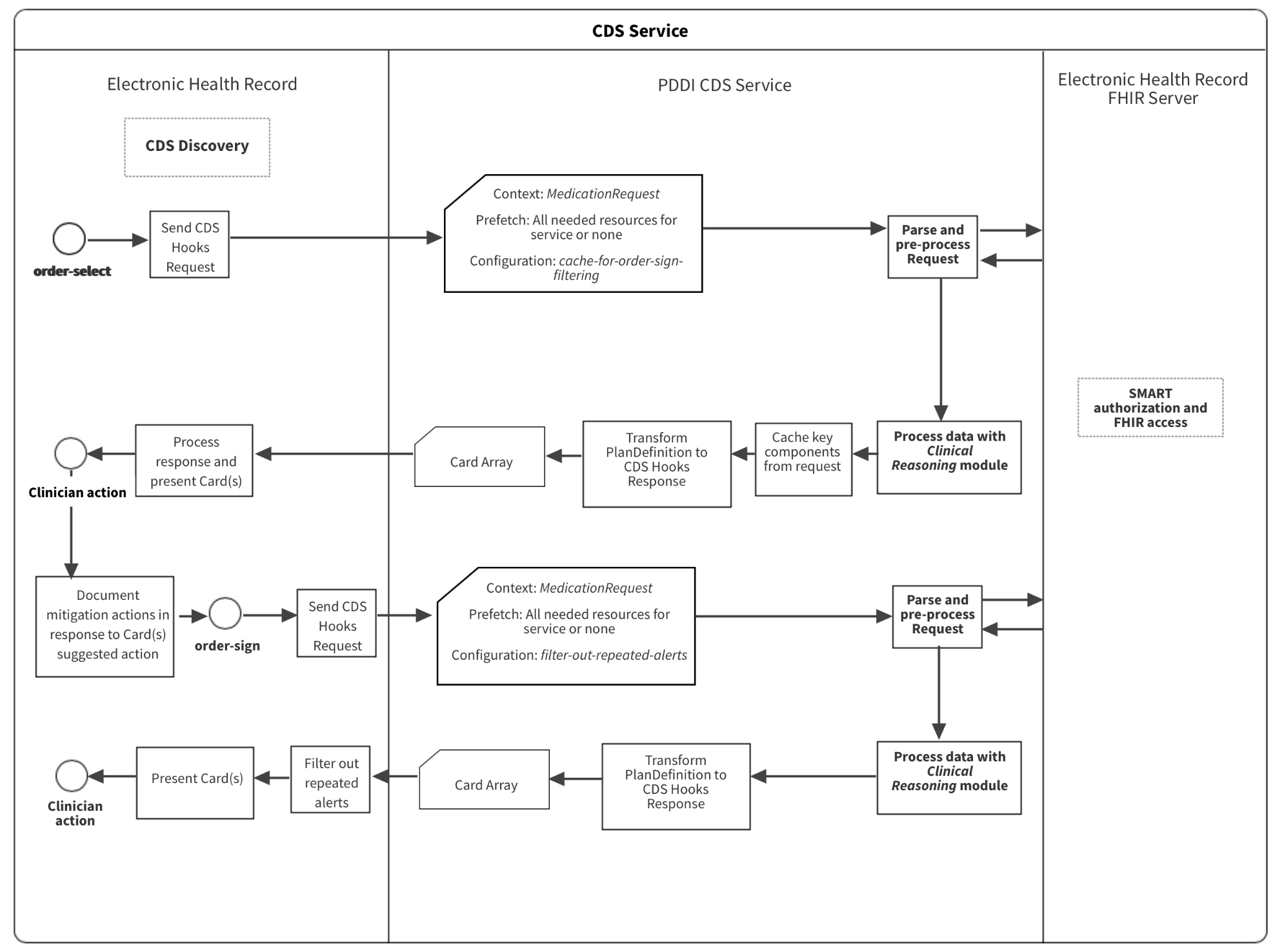
Figure 1 depicts hook triggers for a medication prescribing example. The implementation follows the CDS Hooks order-select and CDS Hooks order-sign specifications that define trigger events when a clinician enters a medication and is ready to sign one or more medication orders for a patient. The order-select hook defines the initial trigger at the start of the CPOE workflow. The order-sign hook is among the last workflow events before an order is promoted out of a draft status. Having the option to trigger the CDS service at only one of two different events in the workflow sets PDDI CDS apart from most conventional CDS systems that trigger CDS at the time of order signing. By moving CDS triggers earlier in the order entry workflow (i.e., order-select), clinicians will have actionable information in the middle of their decision-making process. We think that providing information at this stage presents less of a cognitive burden on the clinician and will lead to more effective CDS. Note that it might not be possible to develop CDS Logic to evaluate a candidate order at the "order-select" stage.' In these cases, appropriately, there would be no ability for the EHR to subscribe to a service specific to the drug-drug interaction that triggers at order-select.
PDDI CDS knowledge artifacts.valueset-warfarin.xml
A CDS rule execution engine (service).
The CDS rule execution engine SHOULD be able to process CDS Hooks requests and return CDS Hooks Card responses. In processing a CDS request, it SHOULD also be able to process FHIR data including clinical and terminology resources.
If the CDS rule execution engine does not receive prefetch data in the request it SHOULD query the FHIR server via network call.
It is RECOMMENDED that the rule engine be able to execute CDS rules written in CQL and represented as a FHIR Library resource, either directly or compiled to HL7 Expression Logical Model.
If the engine implements the advanced functionality described in this implementation guide (i.e., coordination between order-select and order-sign to prevent alert duplication) then, it SHOULD support processing of the configuration options described in Extension subsection. If EHR clients do not send the configuration options, the default behavior of the service should be to NOT suppress card responses at order-sign that might duplicate card responses sent at order-select. This is because the EHR client should have an active role in the decision of whether to filter out alert responses.
It is RECOMMENDED that the rule engine not be given permission to access information that is masked from the clinician whose EHR session has triggered the CDS request (aka 'super user' status) unless there is a specific Break the Glass (BTG) procedure that covers such situations. If there a valid BTG procedure that allows the rule engine to access such information, it SHOULD return an information card stating that such a directive is present. The CDS card SHOULD include that the clinician will be held accountable for BTG throughout any related system audit.
An electronic health record (EHR) CDS client.
Prior to a hook trigger and subsequent processes, the EHR SHOULD initiate a CDS Discovery request. The CDS discovery response is for the system and would not be viewed by the clinician.
The EHR SHOULD call the PDDI CDS service by sending an HTTP POST containing a CDS Hooks request (JSON formatted) to the service endpoint (e.g.,http://FHIR.org/PDDI-CDS/warfarin-nsaids-cds). The JSON (CDS Hooks request) SHOULD contain specified information for the hook that was triggered including FHIR server, user, and context. Provision of prefetch data as specified by the CDS service is RECOMMENDED.
If the EHR client is requesting a CDS from an engine implements the advanced functionality described in this implementation guide (i.e., coordination between order-select and order-sign to prevent alert duplication) then, the client SHOULD use the configuration options described in Extension subsection. The purpose of this is so that the EHR client has an active role in the decision to filter out alert responses.
This section contains documentation on how to implement PDDI CDS artifacts from a clinical and technical perspective. Later sections describe implementation details using a specific knowledge artifact example. Structured artifacts that implement the logic and behavior described below are available under Artifacts.
The words SHOULD, SHOULD NOT, REQUIRED, SHALL, SHALL NOT, SHOULD, SHOULD NOT, RECOMMENDED, MAY, AND OPTIONAL are used as defined "Key words for use in Request for Comment (RFC) to Indicate Requirement Levels". S. Bradner. IETF. March 1997. Best Current Practice.
A web service that processes CDS requests using a CDS rule execution engine. The service SHOULD be able to process CDS Hooks requests and return CDS Hooks Card responses.
A web service that processes CDS requests SHOULD be able to process FHIR data including clinical and terminology resources.
The EHR system that sends requests to the service MAY provide access to the service to relevant patient data in the EHR via a FHIR server. EHR systems that do not provide access to addition patient data will potentially receive more limited CDS because the service will only work with data in the context and prefetch fields of CDS Hooks requests.
Here is a list of FHIR tools that might be of interest to implementers:
Local (preferred)
<b> The HAPI links DO NOT work </b> * [HAPI RESTful Server](http://hapifhir.io/doc_rest_server.html)
To invoke the PDDI CDS service, the EHR needs to send a CDS Hooks request at a pre-specified step the workflow process. The CDS service then parses and processes the request to determine if the prescribed medication conflicts with a medication the patient is presumably taking. If this condition is satisfied, the CDS service provides individualized information based on the PDDI knowledge base. While each implementation may employ a slightly different approach to ensure successful integration of the CDS system. Here are several general aspects to assess:
A technical framework for the EHR to interact with the CDS service by
creating and sending CDS Hooks requests
capturing and presenting CDS Hooks card responses
Use of FHIR terminologies (e.g., RxNorm, LOINC) and other FHIR resources
SMART authentication during FHIR server requests
NEED TO ADD SECTION REGARDING EVIDENCE RESOURCE AND EBM ON FHIR
Figure 1 depicts hook triggers for a medication prescribing example. The implementation follows the CDS Hooks order-select and CDS Hooks order-sign specifications that define trigger events when a clinician enters a medication and is ready to sign one or more medication orders for a patient. The order-select hook defines the initial trigger at the start of the CPOE workflow. The order-sign hook is among the last workflow events before an order is promoted out of a draft status. From a clinical and technical perspective, triggering the CDS service at two events in the workflow sets PDDI CDS apart from most conventional CDS systems that trigger CDS at the time of order signing. By moving CDS triggers earlier in the order entry workflow (i.e., order-select), clinicians will have actionable information in the middle of their decision-making process. We think that providing information at this stage presents less of a cognitive burden on the clinician and will lead to more effective CDS.
Note that the current CDS Hook specification does not have a hook to provide the CDS information at an intermediate step between product selection and signing the order.
For technical implementers, the intended role of prefetch is to improve the CDS service performance. This is achieved by minimizing CDS service network calls to external resources such as a FHIR server. When a client program subscribes to the PDDI CDS service, the service SHOULD return a prefetch specification in the response. This specification identifies resources that the PDDI CDS service SHOULD receive upon request. As described below, the prefetch requirements are different for order-select and order-sign services. The ideal scenario for both implementations and services is to send prefetch data with the CDS Hooks request. The implementor has flexibility on when and how to fulfill the prefetch templates (e.g., data in EHR memory or server call), which will likely result in a solution that reduces the burden of the server and improves the CDS service efficiency. If the CDS service does not receive prefetch data in the request it SHOULD query the server via network call.
Implementers need to consider and address security and privacy concerns that might arise when from providing CDS as a service. One thing to consider is if the clinician ordering a drug is not authorized to have access to information masked due to a patient's consent directive that restricts sharing. For example, consider the Warfarin + non-steroidal anti-inflamatory drugs (NSAIDs) Use Case where the clinician selects warfarin for a patient currently prescribed a NSAID and a proton pump inhibitor. It is conceivable that the clinician would not be aware that the patient is also taking a selective serotonin reuptake inhibitor (SSRI) for a major depressive disorder because the patient did not consent to share this information with anyone besides the mental health provider who prescribed the SSRI. Assuming that the FHIR Authorization Server enforces the patient's consent directive not to disclose to the CDS that the patient is taking a SSRI then, the clinician will not be alerted about the PDDI with NSAID. However, the FHIR Authorization Server could also have an organizational policy that authorizes the CDS as a "super user" and permits it to access to information that is masked from an unauthorized clinician. If the CDS service identifies a PDDI that could result from the order selected by the clinician, it could return a CDS Hook card cautioning the clinician of a possible counter-indication, and recommending that the clinician ask the patient about any medications that the patient has not shared. This would fall under a "Break the Glass" (BTG) scenario and would require a special procedure. A similar CDS BTG scenario was demonstrated during the HIMSS 201902 Orlando Consumer Centered Care Planning Interoperability Showcase and is described here. It was sponsored by the HL7 Security and CBCP WGs, VA, Allscripts, Perspecta, MyPatientLink and others. For more information, see https://build.fhir.org/security-labels.html#break-the-glass and https://build.fhir.org/operationoutcome-example-break-the-glass.html.
It is RECOMMENDED that the rule engine not be given permission to access information that is masked from the clinician whose EHR session has triggered the CDS request (aka 'super user' status) unless there is a specific Break the Glass (BTG) procedure that covers such situations. If there a valid BTG procedure that allows the rule engine to access such information, it SHOULD return an information card stating that such a directive is present. The CDS card SHOULD include that the clinician will be held accountable for BTG throughout any related system audit.
The primary motivation for configuration options is to support the advanced functionality of coordinating between order-select and order-sign to prevent alert duplication. Although it might seem reasonable to have the service default to this kind of coordination with no input from the EHR client, we think that there might be potential scenarios where this form of duplication might be desirable. For example, a teaching hospital might have resident physicians go through the order selection process and then have an attending physician sign off on the order. In this situation, having the same CDS Hooks cards returned at order-select and order-sign would not be perceived as a duplication to the attending. There might be other scenarios where repeating cards across the hooks makes sense. Thus, it seems best to have the EHR client some active role in the decision of whether to filter out alert responses. Using configuration options sent from the EHR client to the service provides a way for the client to have a say in how apparent duplication is handled.
Another role for configuration options would be to enable greater specificity of PDDI CDS to a given clinical environment. This is because clinicians and/or groups of clinicians often have specialized knowledge that might lead them to prioritize information about certain PDDIs over others. One of the advantages of PDDI CDS as a service over the conventional approach of triggering alerts using of a general drug interaction knowledge base is an EHR can be more specific about the interactions provided within a specific clinical environment. For example, clinicians working at a psychiatric hospital might be well versed in psychiatric PDDIs and so only interested in PDDI CDS for drugs they know less about. However, there is another level of specificity that might be beneficial beyond the selection of specific drug combinations. For example, a particular clinician or clinical group might desire to only view PDDIs that are regarded as serious. Also, there might be a preference for the amount of detail in the response narrative. These could be handled using configuration options passed from the EHR client to the CDS service. This would likely be a preferred approach to allow for PDDI CDS to be more customized across many different clinical environments using EHR.
This implementation guide discusses a mechanism for providing the CDS service configuration from CDS Hooks requests. The use of this mechanism is required for the advanced functionality of coordinating between order-select and order-sign. There is no requirement to use additional configuration options at this time. Other possibly useful configuration options, such as to filter out non-serious alerts, might be the focus of a future project.
It is critical for the practicing clinicians using the EHR to be consulted with/actively involved in any configuration decisions made related to the CDS service and what alerts to present. This is because the IT implementers at the site be unlikely to have the clinical knowledge to evaluate the potential burdens of “over alerting” vs. the risks of missing important safety messages. Clinicians need to carefully evaluate the potential burdens vs. risks and make a careful decision on CDS configuration.
The CDS Hooks feedback service provides a mechanism for the CDS Service to receive an update from the client on the acceptance or rejection of a suggestion. This is valuable information to enable a service to improve its behavior towards the goal of the end-user having a positive and meaningful experience with the CDS. There are four distinct, possible outcomes for an end user's single interaction with a CDS Hooks suggestion card: suggestion accepted, card ignored, card dismissed without reason, card dismissed with reason. While the feedback mechanism could potentially provide the CDS Service with greater context for coordination between order-select and order-sign card responses, the coordination mechanism described in this IG does not require its use. EHR clients that implement the hook coordination mechanism (see advanced implementation) MAY integrate feedback to inform how the service filters cards. However, this is not a requirement.
order-sign: CDS Service versus EHR ClientThe preferred implementation is to configure the CDS service to filter duplicative response cards previously shown to the prescriber at order-select as demonstrated in the advanced implementation. In order for PDDI CDS to be both sensitive and specific, different contextual factors are sent to the CDS service depending upon the order entry workflow step the clinician is engaged in. At the time of medication selection, a order-select CDS Hook sends medication resources to the CDS service. Later, at the time of order signing, a order-sign CDS Hook sends other contextual resources specific to a PDDI identified from processing order-select. This might include retrospective patient conditions, lab measurements, and other information. One potential advantage of this approach is a reduction the amount of information needed to provide actionable PDDI information to the clinician. The approach might also limit the amount of information the EHR has to provide for an order entry task. For example, if a clinician starts an NSAID order for a patient that was taking warfarin and decides to discontinue the order based on the presented cards, the clinician only needs to read and process medication factors, and the EHR would not display additional patient resources such as age and history of upper gastrointestinal bleed.
This section provides an overview of the processes and components of the PDDI CDS. It is delineated by Basic and Advanced Implementation sections. The Basic Implementation describes the technology specifications, and what structured code is available in this implementation guide. The Advanced Implementation is a target for future iterations to optimize the CDS artifacts.
Prior to a hook trigger and subsequent processes, the EHR SHOULD initiate a CDS Discovery (Figure 2). CDS Discovery is to identify CDS services and obtain associated prefetch templates. A prefetch template is a dictionary of read and search requests for needed resources of a particular service. The PDDI CDS service MAY provide a prefetch template for each service, and the EHR SHOULD populate prefetch templates with relevant patient data for the anticipated CDS Hook request. The CDS discovery response is for the system and would not be viewed by the clinician.
Example 1: EHR request for CDS Discovery
GET http://FHIR.org/PDDI-CDS
Example 2: CDS Discovery response
{
"services": [
{
"hook": "order-select",
"name": "PlanDefinition - Warfarin NSAIDs Recommendation Workflow",
"title": "Warfarin NSAIDs Recommendation",
"extension": {
"configuration-items": [
{
"code": <an identifier for the configuration option>,
"type": <data type of the configuration option, e.g. boolean>,
"name": <human readable name of the configuration option>,
"description": <human readable description of the configuration option>
},
... other configuration options ...
]
},
"id": "warfarin-nsaids-cds-select",
"prefetch": {
"item1": "Patient?_id=",
"item2": "MedicationRequest?patient=&authoredon=ge2019-12-11",
"item3": "MedicationAdministration?patient=&effective-time=ge2019-12-11",
"item4": "MedicationDispense?patient=&whenhandedover=ge2019-12-11",
"item5": "MedicationStatement?patient=&effective=ge2019-12-11",
"item6": "Condition?patient="
}
},
{
"hook": "order-sign",
"name": "PlanDefinition - Warfarin NSAIDs Recommendation Workflow",
"title": "Warfarin NSAIDs Recommendation",
"extension": {
"configuration-items": [
{
"code": <an identifier for the configuration option>,
"type": <data type of the configuration option, e.g. boolean>,
"name": <human readable name of the configuration option>,
"description": <human readable description of the configuration option>
},
... other configuration options ...
]
},
"id": "warfarin-nsaids-cds-sign",
"prefetch": {
"item1": "Patient?_id=",
"item2": "MedicationRequest?patient=&authoredon=ge2019-12-11",
"item3": "MedicationAdministration?patient=&effective-time=ge2019-12-11",
"item4": "MedicationDispense?patient=&whenhandedover=ge2019-12-11",
"item5": "MedicationStatement?patient=&effective=ge2019-12-11",
"item6": "Condition?patient="
}
}
]
}
The Basic Implementation uses the order-sign 1.0 and is a more simplistic approach compared to the Advanced Implementation. The CDS Hooks specification states that order-sign 1.0 fires when a clinician is ready to sign one or more orders for a patient, (including orders for medications, procedures, labs and other orders). This hook is among the last workflow events before an order is promoted out of a draft status. The context contains all order details, such as dose, quantity, route, etc, although the order has not yet been signed and therefore still exists in a draft status. Use this hook when your service requires all order details, and the clinician will accept recommended changes. Since EHR platforms may have different discrete steps in the order entry process, the implementor decides what action (e.g., selecting a medication product, accepting order completion) triggers the CDS Hooks request.
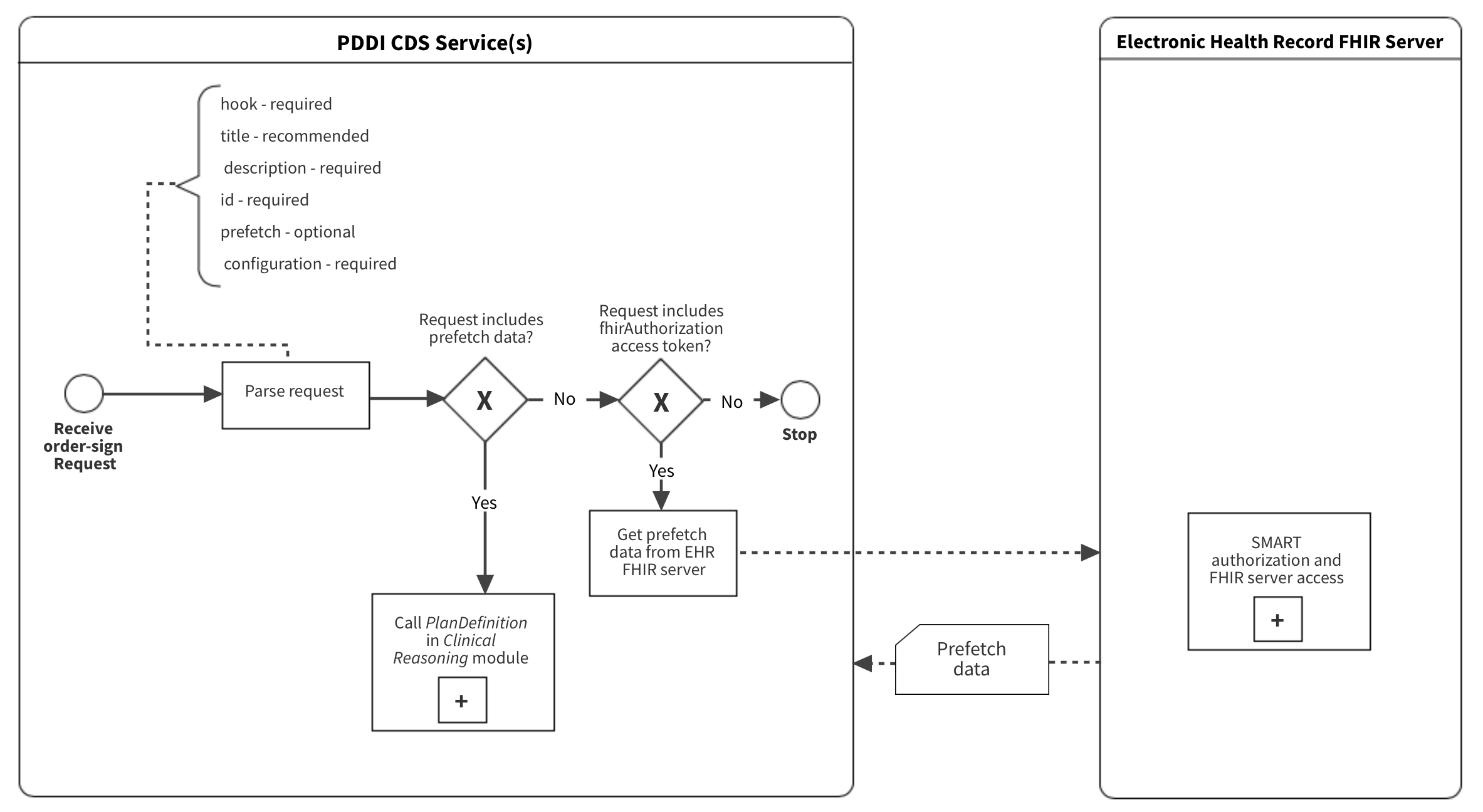
The process for a unique instance of PDDI CDS begins with the user triggering a CDS Hooks request (i.e., order-sign) and ends with the user's action in response to the Card response suggestion(s) (Figure 3). The parse and pre-process subprocess is to determine if a FHIR server query needed. The Clinical Reasoning module evaluates the complete request and creates information to send back the the EHR. The event subprocesses may occur in response to a specific instance (i.e., SMART authorization and FHIR access) or asynchronous of the specific instance (i.e., CDS Discovery).
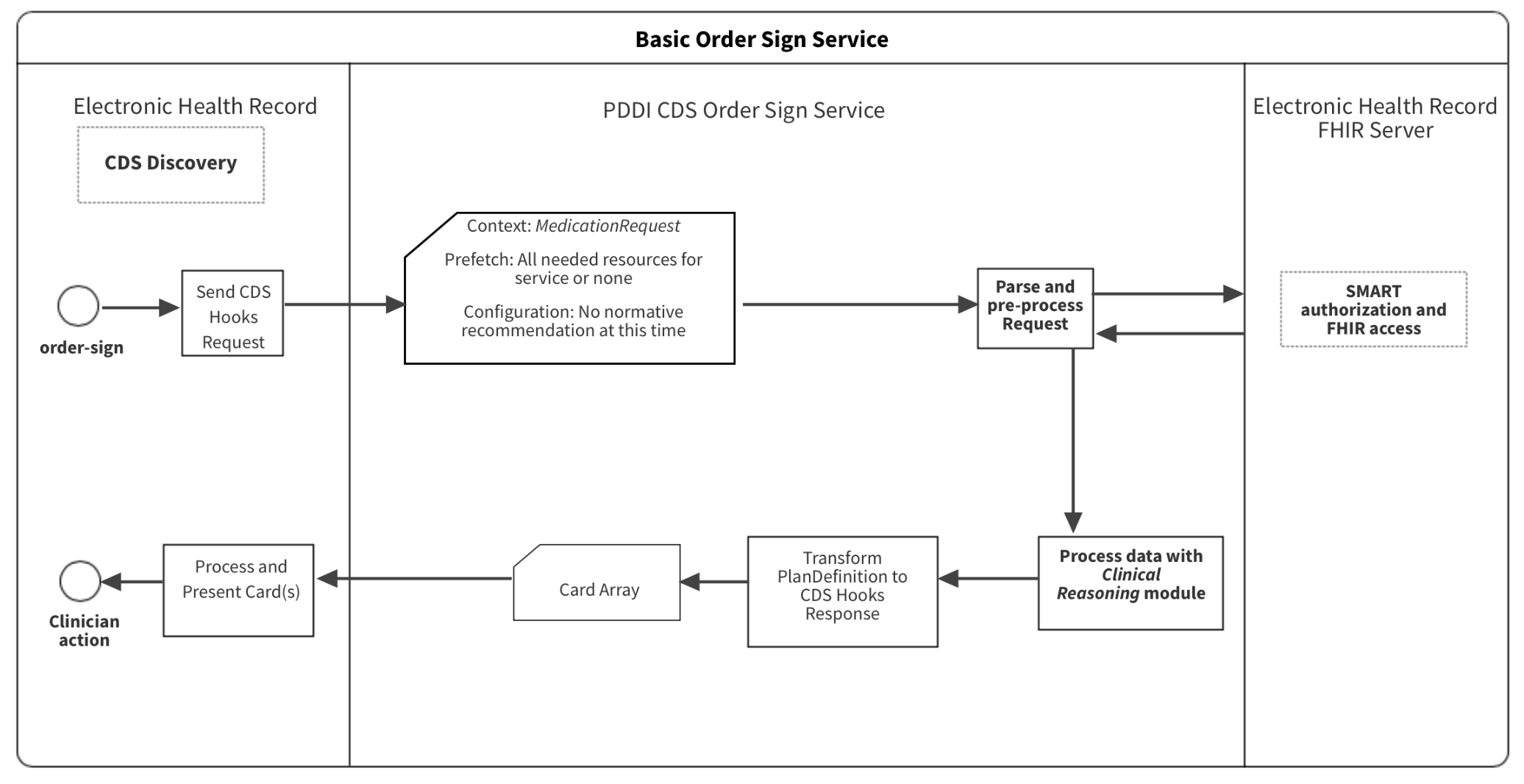
The PDDI CDS artifacts use the current HL7 CDS Hooks specification. The CDS Hooks standard defines the data structure to facilitate communication between the EHR and the CDS service through a RESTful API request and response. This allows patient data to be sent and received by the EHR at intervals that better align with clinical workflows – further leveraging FHIR and SMART applications at the point of care. CDS Hooks instances include CDS Discovery, EHR requests and CDS service response. The context and prefetch are two key elements of the CDS Hook request that contain patient information. The context element contains data that is task and hook-specific. The prefetch element contains patient-specific information that is relevant to the context data and the invoked CDS service. The CDS Hooks response is a set of Cards. The Cards contain general information, suggested actions, and display indicators in a structured format for the EHR to process and display. The CDS Discovery of the CDS Hooks specification delineates information that the CDS service is to provide to the EHR.
Note: The HL7 specification for decision support does not require that the CDS service process CDS Hooks. This implementation guide requires their use because CDS Hooks should provide simplicity and specific orientation for CPOE workflow integration.
The EHR SHOULD call the PDDI CDS service by sending an HTTP POST containing JSON to the service endpoint (e.g.,http://FHIR.org/PDDI-CDS/warfarin-nsaids-cds). The JSON (CDS Hooks request) SHOULD contain specified information for the hook that was triggered, FHIR server, user, context, and prefetch.
Context
The context element of a CDS Hooks request contains contextual data for the current task and is specified below. For example, the order-sign hook specifies the context SHOULD include the medication product (i.e., medication element of the MedicationRequest resource) of the order in process.
order-sign 1.0.
| Field | Optionality | Prefetch Token | Type | Description |
|---|---|---|---|---|
userId |
REQUIRED | Yes | string | The id of the current user. For this hook, the user is expected to be of type Practitioner. For example, Practitioner/123Describe |
patientId |
REQUIRED | Yes | string | The FHIR Patient.id of the current patient in context |
encounterId |
OPTIONAL | Yes | string | The FHIR Encounter.id of the current encounter in context |
draftOrders |
REQUIRED | No | object | object R4 - FHIR Bundle of draft MedicationRequest resource for the current order entry task |
Extension
PDDI Configuration Items
The CDS Service MAY process configuration options sent as within an extension resource with the CDS Hooks request in the field configuration-items. At the present time, there are no standard configuration options for the basic implementation of PDDI CDS. Balloting such options as a standard is for future work. While not a recommendation, some examples can be shown. One example would be a configuration such as alert-non-serious that accepts accepts a Boolean value indicating to the CDS service if it should provide alerts for PDDIs that have an indicator other than 'serious'. Another example would be a configuration such as show-evidence-support indicating to the CDS service that it should provide more detailed evidence support for its alerts.
Prefetch
The prefetch element contains patient data that is provided by the EHR upon submission of the CDS Hook to the CDS service. The CDS service SHOULD provide the EHR with a prefetch template at the time of service discovery. The prefetch element MAY specify patient data other than medications for the purpose of individualizing the CDS logic and response. The prefetch query SHOULD be designed to obtain data for the patient indicated by the context patientID. The CDS service SHOULD then compare the context medication to the patient's current medications in the prefetch element.
Note: For simplicity, this implementation guide uses the term "prefetch" regardless of whether the EHR supplies the data prior to a hook request or if it is queried by the CDS service as a post-hoc FHIR server request.
CDS Hooks Request Example
Bundle
A Bundle is a FHIR resource that groups resources into a single instance, which is ideal for messaging with CDS Hooks, storing a collection of resources obtained on CDS Discovery, and providing flexibility in using the collections as a persistent instance. PDDI CDS implementors SHOULD use the bundle resource for certain context elements and all prefetch resources. For each prefetch template query, a Bundle SHOULD be created to group the resources. A prefetch element MAY contain several Bundle resources with several other resources grouped within.
A FHIR server request by the CDS service is necessary in the event the request prefetch element is empty. While the prefetch element is OPTIONAL, it SHOULD NOT be partially fulfilled. The post-hoc FHIR server query is performed at the parse and pre-process phase shown in Figure 4. To accomplish a FHIR server request, the server URL and the OAuth authorization token (i.e. fhirServer, fhirAuthorization) SHOULD be provided in the CDS Hooks request.
The CDS service response is a Card array. Each Card has specified attributes that map to the core elements of the minimal information model (e.g., summary = Drugs Involved). Each Card has a suggestions array and each suggestion has an action array. The Card indicator element dictates how the EHR presents the alert (e.g., indicator = "critical" could be a modal alert).
Example 3: CDS Hooks Response
{
"cards": [
{
"summary": "Potential drug-drug interaction between naproxen 500mg tablet and warfarin 5mg tablet",
"indicator": "critical",
"detail": "Non-steroidal anti-inflammatory drugs (NSAIDs) have antiplatelet effects which increase the bleeding risk when combined with oral anticoagulants such as warfarin.",
"source": {
"label": "Potential Drug-Drug Interaction CDS",
"suggestions": [
{
"label": "Assess risk and take action if necessary",
"actions": [
{
"type": "create",
"description": "If the NSAID is being used as an analgesic or antipyretic, it would be prudent to use an alternative such as acetaminophen.",
"resource": {
"APAP-order": "MedicationRequest"
}
}
]
}
]
}
},
{
"summary": "Patient is taking omeprazole 20mg daily",
"indicator": "info",
"detail": "Proton pump inhibitors and misoprostol may reduce the risk of UGIB in patients receiving NSAIDs and warfarin.",
"source": {
"label": "Potential Drug-Drug Interaction CDS"
} ...
snipped for brevity
Card Display Example
filter-out-repeated-alerts)
{
"cards": [
{
"summary": "Potential Drug-Drug Interaction between warfarin (Warfarin Sodium 0.5 MG Oral Tablet) and NSAID (Ketorolac Tromethamine 10 MG Oral Tablet).",
"indicator": "warning",
"detail": "Increased risk of bleeding. \nBleeding is a serious potential clinical consequence because it can result in death, life-threatening hospitalization, and disability. \nNon-steroidal anti-inflammatory drugs (NSAIDs) have antiplatelet effects which increase the bleeding risk when combined with oral anticoagulants such as warfarin. The antiplatelet effect of NSAIDs lasts only as long as the NSAID is present in the circulation, unlike aspirin’s antiplatelet effect, which lasts for up to 2 weeks after aspirin is discontinued. NSAIDs also can cause peptic ulcers and most of the evidence for increased bleeding risk with NSAIDs plus warfarin is due to upper gastrointestinal bleeding (UGIB). \nunknown. \n unknown.",
"source": {
"label": "Warfarin-NSAIDs clinical decision support algorithm",
"url": "https://ddi-cds.org/warfarin-nsaids/"
},
"suggestions": [
{
"label": "Assess risk and take action if necessary.",
"actions": [
{
"type": "delete",
"description": "If the NSAID is being used as an analgesic or antipyretic, it would be prudent to use an alternative such as acetaminophen. In some people, acetaminophen can increase the anticoagulant effect of warfarin, so monitor the INR if acetaminophen is used in doses over 2 g/day for a few days. For more severe pain consider short-term opioids in place of the NSAID."
}
]
},
{
"label": "Substitute NSAID (Ketorolac Tromethamine 10 MG Oral Tablet) with APAP (Acetaminophen 325 MG Oral Tablet).",
"actions": [
{
"type": "create",
"description": "Order for APAP <2g per day (APAP 500 mg every 4-6 hours prn).",
"resource": {
"resourceType": "MedicationRequest",
"id": "3f6b9b43-9354-4512-9883-a915417e2936",
"intent": "order",
"medicationCodeableConcept": {
"coding": [
{
"system": "http://www.nlm.nih.gov/research/umls/rxnorm",
"code": "313782",
"display": "Acetaminophen 325 MG Oral Tablet"
}
],
"text": "Acetaminophen 325 MG Oral Tablet"
},
"subject": {
"reference": "f101"
}
}
}
]
},
{
"label": "Substitute NSAID (Ketorolac Tromethamine 10 MG Oral Tablet) with APAP (Acetaminophen 500 MG Oral Tablet).",
"actions": [
{
"type": "create",
"description": "Order for APAP <2g per day (APAP 500 mg every 4-6 hours prn).",
"resource": {
"resourceType": "MedicationRequest",
"id": "d54e75a7-90ce-4ee7-90b6-63333c052648",
"intent": "order",
"medicationCodeableConcept": {
"coding": [
{
"system": "http://www.nlm.nih.gov/research/umls/rxnorm",
"code": "198440",
"display": "Acetaminophen 500 MG Oral Tablet"
}
],
"text": "Acetaminophen 500 MG Oral Tablet"
},
"subject": {
"reference": "f101"
}
}
}
]
}
]
},
{
"summary": "Patient is not taking a proton pump inhibitor or misoprostol.",
"indicator": "critical",
"detail": "Proton pump inhibitors and misoprostol may reduce the risk of UGIB in patients receiving NSAIDs and warfarin.",
"source": {
"label": "Warfarin-NSAIDs clinical decision support algorithm",
"url": "https://ddi-cds.org/warfarin-nsaids/"
},
"suggestions": [
{
"label": "Use only if benefit outweighs risk."
}
]
},
{
"summary": "Patient is 65 y/o or does have a history of upper gastrointestinal bleed (\"Acute duodenal ulcer with hemorrhage\" and 2020-03-01).",
"indicator": "warning",
"detail": "Patients with a history of UGIB or peptic ulcer may have an increased risk of UGIB from this interaction. The extent to which older age is an independent risk factor for UGIB due to these interactions is not firmly established, but UGIB in general is known to increase with age.",
"source": {
"label": "Warfarin-NSAIDs clinical decision support algorithm",
"url": "https://ddi-cds.org/warfarin-nsaids/"
},
"suggestions": [
{
"label": "Use only if benefit outweighs risk."
}
]
},
{
"summary": "Patient is not concomitantly taking systemic corticosteroids, aldosterone antagonist, or high dose or multiple NSAIDs.",
"indicator": "info",
"detail": "Both corticosteroids and aldosterone antagonists have been shown to subsetantially increase the risk of UGIB in patients on NSAIDs, with relative risks of 12.8 and 11 respectively compared to a risk of 4.3 with NSAIDs alone (Masclee et al. Gastroenterology 2014; 147:784-92.)",
"source": {
"label": "Warfarin-NSAIDs clinical decision support algorithm",
"url": "https://ddi-cds.org/warfarin-nsaids/"
},
"suggestions": [
{
"label": "Assess risk and take action if necessary."
}
]
}
]
}
filter-out-repeated-alerts)
{
"cards": [
{
"summary": "Potential Drug-Drug Interaction between digoxin (Digoxin 0.2 MG Oral Capsule) and cyclosporine (Cyclosporine 100 MG)",
"indicator": "warning",
"detail": "Increased risk of digoxin toxicity. Assess risk and take action if necessary. \nDigoxin toxicity is potentially serious. The clinical consequences may include anorexia, nausea, vomiting, visual changes, and cardiac arrhythmias. \nThe mechanism of this interaction appears to be mediated through P-glycoprotein inhibition by cyclosporine. P-glycoprotein is a major transporter for digoxin efflux. \nunknown. \nunknown.",
"source": {
"label": "Potential Drug-Drug Interaction Clinical Decision Support",
"url": "http://hl7.org/fhir/ig/PDDI-CDS"
},
"suggestions": [
{
"label": "Consultation",
"actions": [
{
"type": "create",
"description": "Request communication with digoxin prescriber",
"resource": {
"resourceType": "ProcedureRequest",
"id": "70ef559c-a02d-463d-8505-9beb9c2629c3",
"status": "draft",
"intent": "order",
"code": {
"coding": [
{
"system": "http://snomed.info/sct",
"code": "11429006",
"display": "Consultation"
}
],
"text": "Consultation"
},
"subject": {
"reference": "f001"
}
}
}
]
},
{
"label": "Cancel digoxin",
"actions": [
{
"type": "delete",
"description": "Discontinue digoxin order"
}
]
}
]
},
{
"summary": "Patient does not have digoxin level on record within the last 30 days. ",
"indicator": "warning",
"detail": "Initiating cyclosporine is expected to increase digoxin levels. For patients without a reliable plasma digoxin concentration in normal range, use only if benefits outweight risks. Extreme caution and close monitoring is necessary.",
"source": {
"label": "Potential Drug-Drug Interaction Clinical Decision Support",
"url": "http://hl7.org/fhir/ig/PDDI-CDS"
},
"suggestions": [
{
"label": "Digoxin Level",
"actions": [
{
"type": "create",
"description": "Order digoxin trough within 24 hours from the initiation of cyclosporine",
"resource": {
"resourceType": "ProcedureRequest",
"id": "79d64211-25f6-4e8c-babe-856816127d1b",
"status": "draft",
"intent": "order",
"code": {
"coding": [
{
"system": "http://snomed.info/sct",
"code": "269872007",
"display": "Serum digoxin measurement"
}
],
"text": "Serum digoxin measurement"
},
"subject": {
"reference": "f001"
}
}
}
]
},
{
"label": "New Digoxin",
"actions": [
{
"type": "create",
"description": "Preemptively reduce digoxin dose with new order ",
"resource": {
"resourceType": "MedicationRequest",
"id": "3c428362-5646-4131-9f96-937a7df5dbf4",
"intent": "order",
"medicationCodeableConcept": {
"coding": [
{
"system": "http://www.nlm.nih.gov/research/umls/rxnorm",
"code": "315819",
"display": "Digoxin 0.125 MG"
}
],
"text": "Digoxin 0.125 MG"
},
"subject": {
"reference": "f001"
}
}
}
]
}
],
"links": [
{
"label": "digoxin-cyclosporine PDDI knowledge artifact",
"url": "http://hl7.org/fhir/ig/PDDI-CDS/derived-from#digoxin-cyclosporine-knowledge-artifact"
},
{
"label": "(Dorian et al. Clin Invest Med 1988; 11(2):108-112) ",
"url": "http://hl7.org/fhir/ig/PDDI-CDS/citation#dorian1988"
},
{
"label": "(Dorian et al. Transplant Proc. 1987; 19(1):1825-1827)",
"url": "http://hl7.org/fhir/ig/PDDI-CDS/citation#dorian#1987"
}
]
},
{
"summary": "Within 100 days, the patient has had electrolyte and serum creatinine levels checked, and they are not on a potassium sparing or loop diuretic.",
"indicator": "info",
"detail": "(Potassium: 3.6mEq/L and 2020-04-28)\n (Magnesium: 0.8mmol/L and 2020-04-28)\n (Calcium: 8.6mg/dL and 2020-04-28)\n",
"source": {
"label": "Potential Drug-Drug Interaction Clinical Decision Support",
"url": "http://hl7.org/fhir/ig/PDDI-CDS"
},
"suggestions": [
{
"label": "Serum Creatinine",
"actions": [
{
"type": "create",
"description": "Order for serum creatinine",
"resource": {
"resourceType": "ProcedureRequest",
"id": "85d53af2-22ec-4441-8ecf-f71879779f2a",
"status": "draft",
"intent": "order",
"code": {
"coding": [
{
"system": "http://snomed.info/sct",
"code": " 313822004",
"display": "Corrected serum creatinine"
}
],
"text": "Serum Creatinine"
},
"subject": {
"reference": "f001"
}
}
}
]
},
{
"label": "Electrolyte Panel",
"actions": [
{
"type": "create",
"description": "Order for electrolyte panel",
"resource": {
"resourceType": "ProcedureRequest",
"id": "8c6514e3-1d47-47b6-87b3-fc53ce8f6eb2",
"status": "draft",
"intent": "order",
"code": {
"coding": [
{
"system": "http://snomed.info/sct",
"code": "271236005",
"display": "Serum potassium level"
},
{
"system": "http://snomed.info/sct",
"code": "312475002",
"display": "Plasma magnesium level"
},
{
"system": "http://snomed.info/sct",
"code": "390963002",
"display": "Plasma calcium level"
}
],
"text": "Electrolyte Panel"
},
"subject": {
"reference": "f001"
}
}
}
]
}
],
"links": [
{
"label": "digoxin-cyclosporine PDDI knowledge artifact",
"url": "http://hl7.org/fhir/ig/PDDI-CDS/derived-from#digoxin-cyclosporine-knowledge-artifact"
},
{
"label": "(Lip et al. Postgrad Med J. 1993; 69(811):337)",
"url": "http://hl7.org/fhir/ig/PDDI-CDS/citation#lip1993"
},
{
"label": "(Digoxin-FDA [prescribing information] NDA 20405/S-004)",
"url": "http://hl7.org/fhir/ig/PDDI-CDS/citation#nda20405"
}
]
}
]
}
The Advanced Implementation is a proposed target to optimize PDDI CDS artifacts. It builds on the Basic Implementation; however, implementors SHOULD select either Basic or Advanced Implementation and not both. This section does not provide a comprehensive overview of the implementation but highlights deviations from the Basic Implementation above.
Differences between the Basic and Advanced Implementations include:
Defining two CDS Hooks triggers in CPOE workflow (i.e., order-select and order-sign)
Creating a order-select specification
Modify order-sign specification
Creating separate but coordinated Order Select and Order Sign Services
Note: The Advanced Implementation requires two separate, but coordinated, services for standards' precision, logic flexibility, and to avoid the need for CDS service state.
Different contextual factors are available and needed at different times during the medication order process (Figure 5). To align clinicians' information needs with PDDI information, the Advanced Implementation defines two separate hook trigger events in the medication order workflow:
Selecting a drug product to include in medication order (order-select)
Accepting or signing a single medication order (order-sign)
Coordinating the Order Select Service with the Order Sign Service is a key aspect of the Advanced Implementation. Figure 6 depicts the summary of operations that coordinates the Order Select and Order Sign Services.
{
"services": [
{
"hook": "order-select",
"name": "PlanDefinition - Warfarin NSAIDs Recommendation Workflow",
"title": "Warfarin NSAIDs Recommendation",
"extension": {
"configuration-items": [
{
"code": <an identifier for the configuration option>,
"type": <data type of the configuration option, e.g. boolean>,
"name": <human readable name of the configuration option>,
"description": <human readable description of the configuration option>
},
... other optional configuration options ...
]
},
"id": "warfarin-nsaids-cds-select",
"prefetch": {
"item1": "Patient?_id=",
"item2": "MedicationRequest?patient=&authoredon=ge2019-12-11",
"item3": "MedicationAdministration?patient=&effective-time=ge2019-12-11",
"item4": "MedicationDispense?patient=&whenhandedover=ge2019-12-11",
"item5": "MedicationStatement?patient=&effective=ge2019-12-11",
"item6": "Condition?patient="
}
},
{
"hook": "order-sign",
"name": "PlanDefinition - Warfarin NSAIDs Recommendation Workflow",
"title": "Warfarin NSAIDs Recommendation",
"extension": {
"configuration-items": [
{
"code": <an identifier for the configuration option>,
"type": <data type of the configuration option, e.g. boolean>,
"name": <human readable name of the configuration option>,
"description": <human readable description of the configuration option>
},
... other configuration options ...
]
},
"id": "warfarin-nsaids-cds-sign",
"prefetch": {
"item1": "Patient?_id=",
"item2": "MedicationRequest?patient=&authoredon=ge2019-12-11",
"item3": "MedicationAdministration?patient=&effective-time=ge2019-12-11",
"item4": "MedicationDispense?patient=&whenhandedover=ge2019-12-11",
"item5": "MedicationStatement?patient=&effective=ge2019-12-11",
"item6": "Condition?patient="
}
}
]
}
The Advanced Implementation specifies the use of both the order-select and order-sign CDS Hooks during a single medication order task.
Context
The context element of the order-select CDS Hooks request is identical to the order-sign specification used in the Basic Implementation. For details on the specifications are below.
order-select 1.0
| Field | Optionality | Prefetch Token | Type | Description |
|---|---|---|---|---|
userId |
REQUIRED | Yes | string | The id of the current user. For this hook, the user is expected to be of type Practitioner. For example, Practitioner/123Describe |
patientId |
REQUIRED | Yes | string | The FHIR Patient.id of the current patient |
encounterId |
OPTIONAL | Yes | string | The FHIR Encounter.id of the current encounter |
selections |
REQUIRED | No | array | The FHIR id of the newly selected order(s). The selections field references FHIR resources in the draftOrders Bundle. For example, MedicationRequest/103. |
draftOrders |
REQUIRED | No | object | R4 - FHIR Bundle of draft MedicationRequest resource for the current order entry task |
order-sign 1.0
| Field | Optionality | Prefetch Token | Type | Description |
|---|---|---|---|---|
userId |
REQUIRED | Yes | string | The id of the current user. For this hook, the user is expected to be of type Practitioner. For example, Practitioner/123Describe |
patientId |
REQUIRED | Yes | string | The FHIR Patient.id of the current patient in context |
encounterId |
OPTIONAL | Yes | string | The FHIR Encounter.id of the current encounter in context |
draftOrders |
REQUIRED | No | object | R4 - FHIR Bundle of draft MedicationRequest resource for the current order entry task |
Extension
PDDI Configuration Items
The CDS Service SHOULD process configuration options sent as within an extension resource with the CDS Hooks request in the field configuration-items. There are two standard configuration options that the service and client SHOULD use for coordination during PDDI CDS: cache-for-order-sign-filtering (only used in order-select), filter-out-repeated-alerts (only used in order-sign). All of these configuration options accept Boolean values and are required for the advanced implementation. The cache-for-order-sign-filtering option is used to cache the medication resource during order-select and is used as a reference during order-sign if filter-out-repeated-alerts is set to TRUE. The filter-out-repeated-alerts option is used to hide card results if they were shown in the order-select results.
At the present time, there are no other standard configuration options for the basic implementation of PDDI CDS. Balloting such options as a standard is for future work. While not a recommendation, some examples can be shown. One example would be a configuration such as alert-non-serious that accepts accepts a Boolean value indicating to the CDS service if it should provide alerts for PDDIs that have an indicator other than 'serious'. Another example would be a configuration such as show-evidence-support indicating to the CDS service that it should provide more detailed evidence support for its alerts.
Prefetch
The order entry task is split into two separate CDS Hooks events (i.e., services). The prefetch template for the order-select service SHOULD include medication resources but could include Condition or other resources important for the service to assess for PDDIs.
CDS Hooks Request Example
The parse and pre-process event for a order-select request in the Advanced Implementation is identical to what occurs with order-sign for the Basic Implementation. Processing of order-sign for the Advanced Implementation service is slightly different. During the parse and pre-process phase the CDS service checks the medication that was finally ordered against the medication that was cached during order-select if cache-for-order-sign-filtering was set to TRUE. If filter-out-repeated-alerts is also set to TRUE during order-sign then repeated alert cards will not be returned.
Example: Advanced – CDS Hooks Response
{
"cards": [
{
"summary": "Potential drug-drug interaction between naproxen 500mg tablet and warfarin 5mg tablet",
"indicator": "critical",
"detail": "Non-steroidal anti-inflammatory drugs (NSAIDs) have antiplatelet effects which increase the bleeding risk when combined with oral anticoagulants such as warfarin.",
snipped for brevity
Card Display Example
filter-out-repeated-alerts){
"cards": [
{
"summary": "Potential Drug-Drug Interaction between warfarin (Warfarin Sodium 0.5 MG Oral Tablet) and NSAID (Ketorolac Tromethamine 10 MG Oral Tablet).",
"indicator": "warning",
"detail": "Increased risk of bleeding. \nBleeding is a serious potential clinical consequence because it can result in death, life-threatening hospitalization, and disability. \nNon-steroidal anti-inflammatory drugs (NSAIDs) have antiplatelet effects which increase the bleeding risk when combined with oral anticoagulants such as warfarin. The antiplatelet effect of NSAIDs lasts only as long as the NSAID is present in the circulation, unlike aspirin’s antiplatelet effect, which lasts for up to 2 weeks after aspirin is discontinued. NSAIDs also can cause peptic ulcers and most of the evidence for increased bleeding risk with NSAIDs plus warfarin is due to upper gastrointestinal bleeding (UGIB). \nunknown. \n unknown.",
"source": {
"label": "Warfarin-NSAIDs clinical decision support algorithm",
"url": "https://ddi-cds.org/warfarin-nsaids/"
},
"suggestions": [
{
"label": "Assess risk and take action if necessary.",
"actions": [
{
"type": "delete",
"description": "If the NSAID is being used as an analgesic or antipyretic, it would be prudent to use an alternative such as acetaminophen. In some people, acetaminophen can increase the anticoagulant effect of warfarin, so monitor the INR if acetaminophen is used in doses over 2 g/day for a few days. For more severe pain consider short-term opioids in place of the NSAID."
}
]
},
{
"label": "Substitute NSAID (Ketorolac Tromethamine 10 MG Oral Tablet) with APAP (Acetaminophen 325 MG Oral Tablet).",
"actions": [
{
"type": "create",
"description": "Order for APAP <2g per day (APAP 500 mg every 4-6 hours prn).",
"resource": {
"resourceType": "MedicationRequest",
"id": "3f6b9b43-9354-4512-9883-a915417e2936",
"intent": "order",
"medicationCodeableConcept": {
"coding": [
{
"system": "http://www.nlm.nih.gov/research/umls/rxnorm",
"code": "313782",
"display": "Acetaminophen 325 MG Oral Tablet"
}
],
"text": "Acetaminophen 325 MG Oral Tablet"
},
"subject": {
"reference": "f101"
}
}
}
]
},
{
"label": "Substitute NSAID (Ketorolac Tromethamine 10 MG Oral Tablet) with APAP (Acetaminophen 500 MG Oral Tablet).",
"actions": [
{
"type": "create",
"description": "Order for APAP <2g per day (APAP 500 mg every 4-6 hours prn).",
"resource": {
"resourceType": "MedicationRequest",
"id": "d54e75a7-90ce-4ee7-90b6-63333c052648",
"intent": "order",
"medicationCodeableConcept": {
"coding": [
{
"system": "http://www.nlm.nih.gov/research/umls/rxnorm",
"code": "198440",
"display": "Acetaminophen 500 MG Oral Tablet"
}
],
"text": "Acetaminophen 500 MG Oral Tablet"
},
"subject": {
"reference": "f101"
}
}
}
]
}
]
},
{
"summary": "Patient is not taking a proton pump inhibitor or misoprostol.",
"indicator": "critical",
"detail": "Proton pump inhibitors and misoprostol may reduce the risk of UGIB in patients receiving NSAIDs and warfarin.",
"source": {
"label": "Warfarin-NSAIDs clinical decision support algorithm",
"url": "https://ddi-cds.org/warfarin-nsaids/"
},
"suggestions": [
{
"label": "Use only if benefit outweighs risk."
}
]
},
{
"summary": "Patient is 65 y/o or does have a history of upper gastrointestinal bleed (\"Acute duodenal ulcer with hemorrhage\" and 2020-03-01).",
"indicator": "warning",
"detail": "Patients with a history of UGIB or peptic ulcer may have an increased risk of UGIB from this interaction. The extent to which older age is an independent risk factor for UGIB due to these interactions is not firmly established, but UGIB in general is known to increase with age.",
"source": {
"label": "Warfarin-NSAIDs clinical decision support algorithm",
"url": "https://ddi-cds.org/warfarin-nsaids/"
},
"suggestions": [
{
"label": "Use only if benefit outweighs risk."
}
]
},
{
"summary": "Patient is not concomitantly taking systemic corticosteroids, aldosterone antagonist, or high dose or multiple NSAIDs.",
"indicator": "info",
"detail": "Both corticosteroids and aldosterone antagonists have been shown to subsetantially increase the risk of UGIB in patients on NSAIDs, with relative risks of 12.8 and 11 respectively compared to a risk of 4.3 with NSAIDs alone (Masclee et al. Gastroenterology 2014; 147:784-92.)",
"source": {
"label": "Warfarin-NSAIDs clinical decision support algorithm",
"url": "https://ddi-cds.org/warfarin-nsaids/"
},
"suggestions": [
{
"label": "Assess risk and take action if necessary."
}
]
}
]
}
filter-out-repeated-alerts){
"cards": [
{
"summary": "An alert was filtered because this request is configured to filter alerts if they were presented previously in response to a prior CDS Hook request.",
"indicator": "info",
"detail": "Since filter-out-repeated-alerts was set to true in this CDS Hook request, the service is filtering out cards that were triggered by the same knowledge artifact when the physician reference display, encounter id, and patient id match between the order-select and order-sign requests.",
"source": {}
}
]
}
filter-out-repeated-alerts){
"cards": [
{
"summary": "Potential Drug-Drug Interaction between digoxin (Digoxin 0.2 MG Oral Capsule) and cyclosporine (Cyclosporine 100 MG)",
"indicator": "warning",
"detail": "Increased risk of digoxin toxicity. Assess risk and take action if necessary. \nDigoxin toxicity is potentially serious. The clinical consequences may include anorexia, nausea, vomiting, visual changes, and cardiac arrhythmias. \nThe mechanism of this interaction appears to be mediated through P-glycoprotein inhibition by cyclosporine. P-glycoprotein is a major transporter for digoxin efflux. \nunknown. \nunknown.",
"source": {
"label": "Potential Drug-Drug Interaction Clinical Decision Support",
"url": "http://hl7.org/fhir/ig/PDDI-CDS"
},
"suggestions": [
{
"label": "Consultation",
"actions": [
{
"type": "create",
"description": "Request communication with digoxin prescriber",
"resource": {
"resourceType": "ProcedureRequest",
"id": "70ef559c-a02d-463d-8505-9beb9c2629c3",
"status": "draft",
"intent": "order",
"code": {
"coding": [
{
"system": "http://snomed.info/sct",
"code": "11429006",
"display": "Consultation"
}
],
"text": "Consultation"
},
"subject": {
"reference": "f001"
}
}
}
]
},
{
"label": "Cancel digoxin",
"actions": [
{
"type": "delete",
"description": "Discontinue digoxin order"
}
]
}
]
},
{
"summary": "Patient does not have digoxin level on record within the last 30 days. ",
"indicator": "warning",
"detail": "Initiating cyclosporine is expected to increase digoxin levels. For patients without a reliable plasma digoxin concentration in normal range, use only if benefits outweight risks. Extreme caution and close monitoring is necessary.",
"source": {
"label": "Potential Drug-Drug Interaction Clinical Decision Support",
"url": "http://hl7.org/fhir/ig/PDDI-CDS"
},
"suggestions": [
{
"label": "Digoxin Level",
"actions": [
{
"type": "create",
"description": "Order digoxin trough within 24 hours from the initiation of cyclosporine",
"resource": {
"resourceType": "ProcedureRequest",
"id": "79d64211-25f6-4e8c-babe-856816127d1b",
"status": "draft",
"intent": "order",
"code": {
"coding": [
{
"system": "http://snomed.info/sct",
"code": "269872007",
"display": "Serum digoxin measurement"
}
],
"text": "Serum digoxin measurement"
},
"subject": {
"reference": "f001"
}
}
}
]
},
{
"label": "New Digoxin",
"actions": [
{
"type": "create",
"description": "Preemptively reduce digoxin dose with new order ",
"resource": {
"resourceType": "MedicationRequest",
"id": "3c428362-5646-4131-9f96-937a7df5dbf4",
"intent": "order",
"medicationCodeableConcept": {
"coding": [
{
"system": "http://www.nlm.nih.gov/research/umls/rxnorm",
"code": "315819",
"display": "Digoxin 0.125 MG"
}
],
"text": "Digoxin 0.125 MG"
},
"subject": {
"reference": "f001"
}
}
}
]
}
],
"links": [
{
"label": "digoxin-cyclosporine PDDI knowledge artifact",
"url": "http://hl7.org/fhir/ig/PDDI-CDS/derived-from#digoxin-cyclosporine-knowledge-artifact"
},
{
"label": "(Dorian et al. Clin Invest Med 1988; 11(2):108-112) ",
"url": "http://hl7.org/fhir/ig/PDDI-CDS/citation#dorian1988"
},
{
"label": "(Dorian et al. Transplant Proc. 1987; 19(1):1825-1827)",
"url": "http://hl7.org/fhir/ig/PDDI-CDS/citation#dorian#1987"
}
]
},
{
"summary": "Within 100 days, the patient has had electrolyte and serum creatinine levels checked, and they are not on a potassium sparing or loop diuretic.",
"indicator": "info",
"detail": "(Potassium: 3.6mEq/L and 2020-04-28)\n (Magnesium: 0.8mmol/L and 2020-04-28)\n (Calcium: 8.6mg/dL and 2020-04-28)\n",
"source": {
"label": "Potential Drug-Drug Interaction Clinical Decision Support",
"url": "http://hl7.org/fhir/ig/PDDI-CDS"
},
"suggestions": [
{
"label": "Serum Creatinine",
"actions": [
{
"type": "create",
"description": "Order for serum creatinine",
"resource": {
"resourceType": "ProcedureRequest",
"id": "85d53af2-22ec-4441-8ecf-f71879779f2a",
"status": "draft",
"intent": "order",
"code": {
"coding": [
{
"system": "http://snomed.info/sct",
"code": " 313822004",
"display": "Corrected serum creatinine"
}
],
"text": "Serum Creatinine"
},
"subject": {
"reference": "f001"
}
}
}
]
},
{
"label": "Electrolyte Panel",
"actions": [
{
"type": "create",
"description": "Order for electrolyte panel",
"resource": {
"resourceType": "ProcedureRequest",
"id": "8c6514e3-1d47-47b6-87b3-fc53ce8f6eb2",
"status": "draft",
"intent": "order",
"code": {
"coding": [
{
"system": "http://snomed.info/sct",
"code": "271236005",
"display": "Serum potassium level"
},
{
"system": "http://snomed.info/sct",
"code": "312475002",
"display": "Plasma magnesium level"
},
{
"system": "http://snomed.info/sct",
"code": "390963002",
"display": "Plasma calcium level"
}
],
"text": "Electrolyte Panel"
},
"subject": {
"reference": "f001"
}
}
}
]
}
],
"links": [
{
"label": "digoxin-cyclosporine PDDI knowledge artifact",
"url": "http://hl7.org/fhir/ig/PDDI-CDS/derived-from#digoxin-cyclosporine-knowledge-artifact"
},
{
"label": "(Lip et al. Postgrad Med J. 1993; 69(811):337)",
"url": "http://hl7.org/fhir/ig/PDDI-CDS/citation#lip1993"
},
{
"label": "(Digoxin-FDA [prescribing information] NDA 20405/S-004)",
"url": "http://hl7.org/fhir/ig/PDDI-CDS/citation#nda20405"
}
]
}
]
}
filter-out-repeated-alerts){
"cards": [
{
"summary": "An alert was filtered because this request is configured to filter alerts if they were presented previously in response to a prior CDS Hook request.",
"indicator": "info",
"detail": "Since filter-out-repeated-alerts was set to true in this CDS Hook request, the service is filtering out cards that were triggered by the same knowledge artifact when the physician reference display, encounter id, and patient id match between the order-select and order-sign requests.",
"source": {}
}
]
}
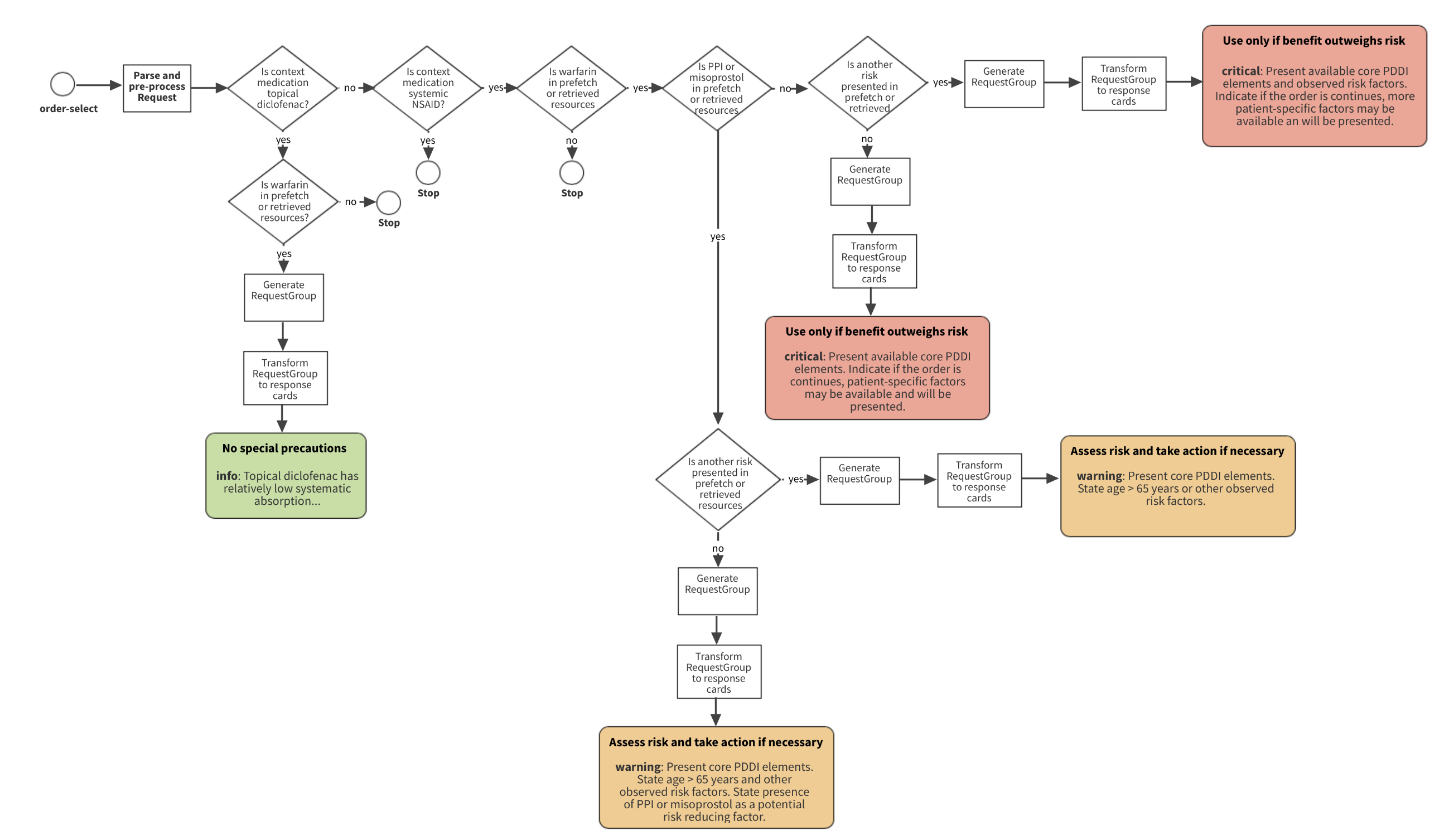
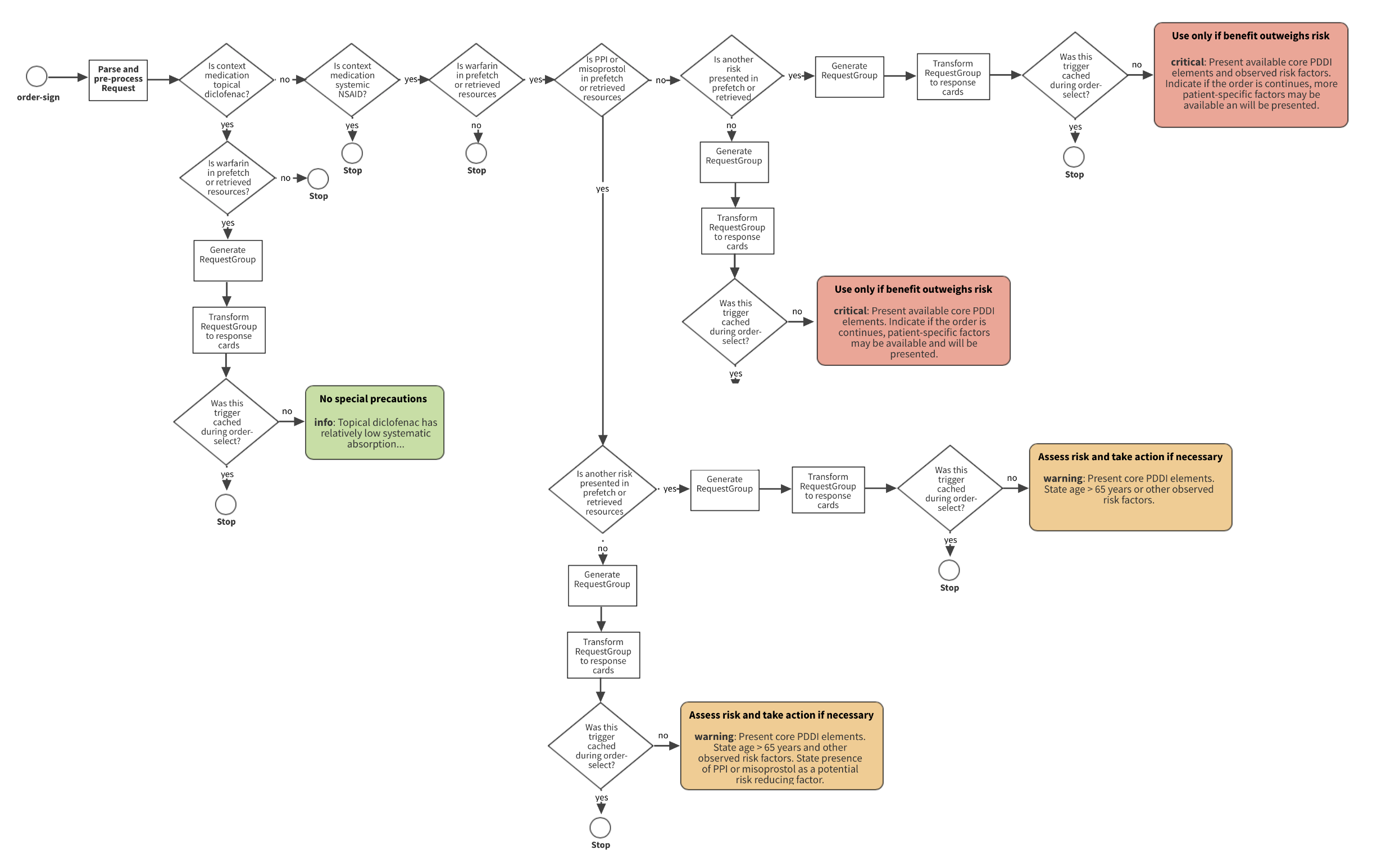
Figure 8 depicts how a PDDI CDS implementer would translate a minimal information model narrative to a semi-structured knowledge artifact. The Basic Implementation uses a single CDS service call and response with the order-sign hook. The decision tree results in three warning indicators (i.e., green, orange, red) and contextual factors that MAY be passed to the clinician. After processing the CDS Hooks order-sign request, the CDS service SHOULD return CDS Hooks Cards that MAY include actions with associated FHIR resources. Figure 9 builds on Figure 8 by depicting a Card display example within the order entry workflow. The decision points, order-sign request, and Card(s) response are discussed further in the sections below.
Many PDDI CDS scenarios have similar drug and patient related decision points. Implementers SHOULD develop CQL artifacts that work in conjunction with the order-sign context and prefetch to support the base decision points. The Warfarin + NSAIDs PDDI exemplar as three main decision blocks that include:
whether the prescribed NSAID is topical diclofenac,
whether the patient is taking a proton pump inhibitor, and
the presence or absence of risk factors involving age, exacerbating medications, and history of upper gastrointestinal bleed
The order-sign request includes context and prefetch elements with FHIR resource attributes or entire resources. The contents of these elements for the Warfarin + NSAIDs CDS artifact are shown below.
Context
Prefetch
Note: The use of multiple medication resources is to ensure a comprehensive capture of medications the patient may be taking. In some cases the implementing institution may only have access to MedicationRequest (prescription order), and in other cases they may have access to several resources for a specific medication intervention (e.g., prescription order from medical office, prescription product picked up from pharmacy). The 100-day look-back period is a general starting point. Implementors SHOULD refine this based on the available data. For example, MedicationAdministration is typically documented in the inpatient setting when a nurse administers a medication. This data source may be a more reliable proxy for blood concentrations and could be used to refine CDS logic.
The CDS Hooks service response supports providing actionable information to clinicians at the time of medication order entry. A response Card has an action element within the suggestion attribute. The action element is defined by three types including create, update, and delete. Depending on the type of action, resources may be provided that facilitate the suggestion. For example, if a suggestion recommends substituting substitute acetaminophen for naproxen, a create action may be used to apply a MedicationRequest for acetaminophen to the current order entry task. The actions, types and associated resources are listed below.
create
updatedelete
Note: These actions are options that SHOULD be customized to an institutions needs and capabilities.
The Advanced Implementation for the Warfarin + NSAIDs artifact is split into two separate hooks and services. Figures 10 and 11 depict the decision tree for warning indicators (i.e., green, orange, red) and contextual factors for both Hooks (i.e., order-select and order-sign). Figure 10 provides a Card display example for each CDS Hooks instance within the order entry workflow. In the provided Card display example, the clinician decided to order the NSAID medication but adds a proton pump inhibitor, in response to the card suggestion. This action results in a downgrade of the response card (i.e., "critical" – red to "warning" – orange).
Context
order-select 1.0.
| Field | Optionality | Prefetch Token | Type | Description |
|---|---|---|---|---|
userId |
REQUIRED | Yes | string | The id of the current user. For this hook, the user is expected to be of type Practitioner. For example, Practitioner/123Describe |
patientId |
REQUIRED | Yes | string | The FHIR Patient.id of the current patient |
encounterId |
OPTIONAL | Yes | string | The FHIR Encounter.id of the current encounter |
selections |
REQUIRED | No | array | The FHIR id of the newly selected order(s). The selections field references FHIR resources in the draftOrders Bundle. For example, MedicationRequest/103. |
draftOrders |
REQUIRED | No | object | R4 - FHIR Bundle of draft MedicationRequest resource for the current order entry task |
order-sign 1.0
| Field | Optionality | Prefetch Token | Type | Description |
|---|---|---|---|---|
userId |
REQUIRED | Yes | string | The id of the current user. For this hook, the user is expected to be of type Practitioner. For example, Practitioner/123Describe |
patientId |
REQUIRED | Yes | string | The FHIR Patient.id of the current patient in context |
encounterId |
OPTIONAL | Yes | string | The FHIR Encounter.id of the current encounter in context |
draftOrders |
REQUIRED | No | object | R4 - FHIR Bundle of draft MedicationRequest resource for the current order entry task |
order-select prefetch
order-sign prefetch
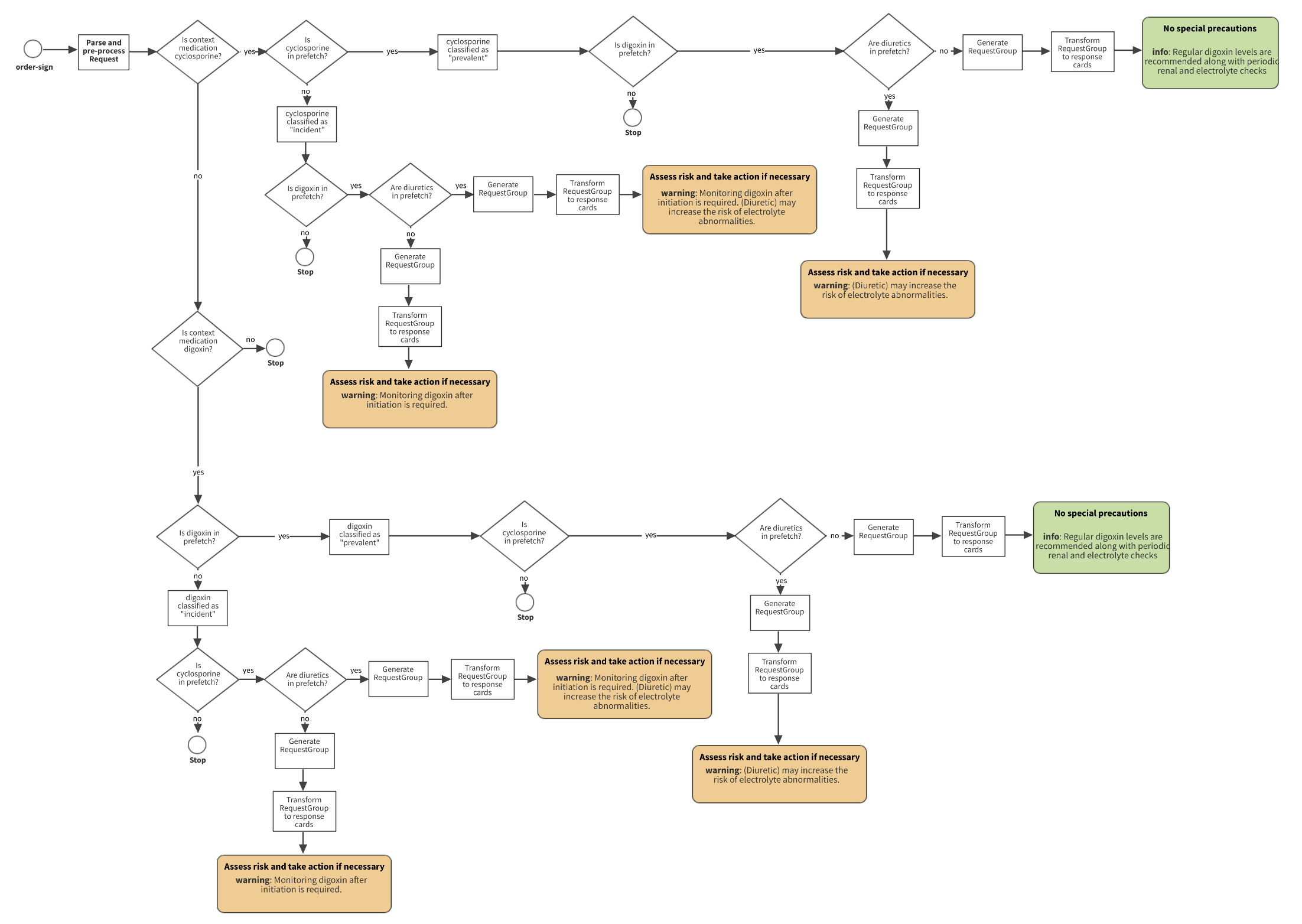
Figure 13 depicts how a PDDI CDS implementer would translate a minimal information model narrative to a semi-structured knowledge artifact. The Basic Implementation uses a single CDS service call and response with the order-sign hook. The decision tree results in three warning indicators (i.e., green, orange, red) and contextual factors that MAY be passed to the clinician. After processing the CDS Hooks order-sign request, the CDS service SHOULD return CDS Hooks Cards that MAY include actions with associated FHIR resources. Figure 14 builds on Figure 13 by depicting a Card display example within the order entry workflow. The decision points, order-sign request, and Card(s) response are discussed further in the sections below.
The Digoxin + Cyclosporine exemplar artifact has two main decision blocks:
whether the patient is taking digoxin and/or cyclosporine at the time of the current order for digoxin or cyclosporine, and
whether the patient has risk factors that may potentiate the risk of digitalis toxicity.
The order-sign request includes context and prefetch elements with FHIR resource attributes or entire resources. The contents of these elements for the Digoxin + Cyclosporine CDS artifact are shown below.
Context
Prefetch
The CDS Hooks service response supports providing actionable information to clinicians at the time of medication order entry. A response Card has an action element within the suggestion attribute. The action element is defined by three types including create, update, and delete. Depending on the type of action, resources may be provided that facilitate the suggestion. For example, if a suggestion recommends substituting acetaminophen for naproxen, a create action may be used to apply a MedicationRequest for acetaminophen to the current order entry task. The actions, types and associated resources are listed below.
create
update
delete
Note: These actions are options that SHOULD be customized to an institutions needs and capabilities.
The Advanced Implementation for the Digoxin + Cyclosporine artifact is split into two separate hooks and services. Figures 15 and 16 depict the decision tree for warning indicators (i.e., green, orange, red) and contextual factors for both Hooks (i.e., order-select and order-sign). Figure 10 provides a Card display example for each CDS Hooks instance within the order entry workflow. In the provided Card display example, the clinician decided to order the NSAID medication but adds a proton pump inhibitor, in response to the card suggestion. This action results in a downgrade of the response card (i.e., "critical" – red to "warning" – orange).
Context
order-select 1.0.
| Field | Optionality | Prefetch Token | Type | Description |
|---|---|---|---|---|
userId |
REQUIRED | Yes | string | The id of the current user. For this hook, the user is expected to be of type Practitioner. For example, Practitioner/123Describe |
patientId |
REQUIRED | Yes | string | The FHIR Patient.id of the current patient |
encounterId |
OPTIONAL | Yes | string | The FHIR Encounter.id of the current encounter |
selections |
REQUIRED | No | array | The FHIR id of the newly selected order(s). The selections field references FHIR resources in the draftOrders Bundle. For example, MedicationRequest/103. |
draftOrders |
REQUIRED | No | object | R4 - FHIR Bundle of draft MedicationRequest resource for the current order entry task |
order-sign 1.0
| Field | Optionality | Prefetch Token | Type | Description |
|---|---|---|---|---|
userId |
REQUIRED | Yes | string | The id of the current user. For this hook, the user is expected to be of type Practitioner. For example, Practitioner/123Describe |
patientId |
REQUIRED | Yes | string | The FHIR Patient.id of the current patient in context |
encounterId |
OPTIONAL | Yes | string | The FHIR Encounter.id of the current encounter in context |
draftOrders |
REQUIRED | No | object | R4 - FHIR Bundle of draft MedicationRequest resource for the current order entry task |
order-select prefetch
order-sign prefetch
The following tables have been created to better conceptualize the various scenarios where message filtering may occur
for the clinician during order-sign. The assumptions used when creating these tables are that cache-for-order-sign-filtering
and filter-out-repeated-alerts for both order-select and order-sign are set to TRUE. During order-select the
following items are cached in order to properly handle message filtering.
selectionsorder-sign)Clinician A calls order-select with 1 medication in draftOrders that triggers a branch of the rules then calls order-sign.
Note: CDS hooks do not couple
indicatorswithsuggestions.
| Indicator for the branch triggered | Service suggested action | Clinician accepts suggested action | Will alert be filtered | Description |
|---|---|---|---|---|
| Info | Create/Update/Delete | FALSE | TRUE | Only message received is non-serious, no action is taken and alert will be filtered on order-sign |
| Info | Create | TRUE | FALSE | If action taken does not trigger a new order-select call, alert will not be filtered on order-sign |
| Info | Update | TRUE | FALSE | If action taken does not trigger a new order-select call, alert will not be filtered on order-sign |
| Info | Delete | TRUE | FALSE | If action taken does not trigger a new order-select call, alert will not be filtered on order-sign |
| Warning | Create/Update/Delete | FALSE | TRUE | Warning message received, no additional action taken, alert will be filtered on order-sign |
| Warning | Create | TRUE | FALSE | If action taken does not trigger a new order-select call, alert will not be filtered on order-sign |
| Warning | Update | TRUE | FALSE | If action taken does not trigger a new order-select call, alert will not be filtered on order-sign |
| Warning | Delete | TRUE | FALSE | If action taken does not trigger a new order-select call, alert will not be filtered on order-sign |
| Critical | Create/Update/Delete | FALSE | TRUE | Critical message received, no additional action taken, alert will be filtered on order-sign |
| Critical | Create | TRUE | FALSE | If action taken does not trigger a new order-select call, alert will not be filtered on order-sign |
| Critical | Update | TRUE | FALSE | If action taken does not trigger a new order-select call, alert will not be filtered on order-sign |
| Critical | Delete | TRUE | FALSE | If action taken does not trigger a new order-select call, alert will not be filtered on order-sign |
Each medication request specified in selections will be cached for message filtering on order-sign, this scenario will operate just as above.
Clinician A goes through an order-select process, for some reason is not able to start the order-sign process immediately. Clinician B then goes through the order-select and order-sign process for the same patient.
| Branch triggered for clinician A | Branch triggered for clinician B | Will alert be filtered | Description |
|---|---|---|---|
| Info | Info | FALSE | Because the clinician IDs are different the alerts will not be filtered on order-sign |
| Warning | Warning | FALSE | Because the clinician IDs are different the alerts will not be filtered on order-sign |
| Critical | Critical | FALSE | Because the clinician IDs are different the alerts will not be filtered on order-sign |
| Info | Warning | FALSE | Because the clinician IDs are different the alerts will not be filtered on order-sign |
| Info | Critical | FALSE | Because the clinician IDs are different the alerts will not be filtered on order-sign |
| Warning | Info | FALSE | Because the clinician IDs are different the alerts will not be filtered on order-sign |
| Warning | Critical | FALSE | Because the clinician IDs are different the alerts will not be filtered on order-sign |
| Critical | Info | FALSE | Because the clinician IDs are different the alerts will not be filtered on order-sign |
| Critical | Warning | FALSE | Because the clinician IDs are different the alerts will not be filtered on order-sign |
Clinician A starts the order-select process, gets interrupted and prevented from beginning the order-sign processes (potential network issues or other problems arise). Clinician A then goes through the order-select process again before completing order-sign.
| Branch triggered for both order-selects | Will alert be filtered | Description |
|---|---|---|
| Info | TRUE | Message filtering is never performed on the messages returned from an order-select call. All messages will be filtered normally on the order-sign call |
| Warning | TRUE | Message filtering is never performed on the messages returned from an order-select call. All messages will be filtered normally on the order-sign call |
| Critical | TRUE | Message filtering is never performed on the messages returned from an order-select call. All messages will be filtered normally on the order-sign call |
Clinician A starts the order-select process with 1 medication in the draft orders that triggers a rule set. Clinician A
then add a second medication to draft orders which triggers a different rule set. Clinician A then begins the order-sign
process with both medications in the draft orders.
| Indicator for the branch triggered (medication 1) | Indicator for the branch triggered (medication 2) | Will alerts be filtered | Description |
|---|---|---|---|
| Info | Info | TRUE | Message filtering will be performed. No change in the ordering clinician, patient, encounter, and knowledge artifact URL. The CDS card is cached as well to ensure repeated messages are not shown even if the rule set that is triggered by each medication is different. |
| Info | Warning | TRUE | Message filtering will be performed. No change in the ordering clinician, patient, encounter, and knowledge artifact URL. The CDS card is cached as well to ensure repeated messages are not shown even if the rule set that is triggered by each medication is different. |
| Info | Critical | TRUE | Message filtering will be performed. No change in the ordering clinician, patient, encounter, and knowledge artifact URL. The CDS card is cached as well to ensure repeated messages are not shown even if the rule set that is triggered by each medication is different. |
| Warning | Info | TRUE | Message filtering will be performed. No change in the ordering clinician, patient, encounter, and knowledge artifact URL. The CDS card is cached as well to ensure repeated messages are not shown even if the rule set that is triggered by each medication is different. |
| Warning | Warning | TRUE | Message filtering will be performed. No change in the ordering clinician, patient, encounter, and knowledge artifact URL. The CDS card is cached as well to ensure repeated messages are not shown even if the rule set that is triggered by each medication is different. |
| Warning | Critical | TRUE | Message filtering will be performed. No change in the ordering clinician, patient, encounter, and knowledge artifact URL. The CDS card is cached as well to ensure repeated messages are not shown even if the rule set that is triggered by each medication is different. |
| Critical | Info | TRUE | Message filtering will be performed. No change in the ordering clinician, patient, encounter, and knowledge artifact URL. The CDS card is cached as well to ensure repeated messages are not shown even if the rule set that is triggered by each medication is different. |
| Critical | Warning | TRUE | Message filtering will be performed. No change in the ordering clinician, patient, encounter, and knowledge artifact URL. The CDS card is cached as well to ensure repeated messages are not shown even if the rule set that is triggered by each medication is different. |
| Critical | Critical | TRUE | Message filtering will be performed. No change in the ordering clinician, patient, encounter, and knowledge artifact URL. The CDS card is cached as well to ensure repeated messages are not shown even if the rule set that is triggered by each medication is different. |
Clinician A completes the order-select process, something prevents them from starting order-sign for a long period of time.
Note: There is currently no time-out period or expiration for cached medications to reset
order-signmessage filtering
| Branch triggered | Time-out set | Will alert be filtered | Description |
|---|---|---|---|
| Info | FALSE | TRUE | Message filtering will be performed as normal |
| Info | TRUE | FALSE | If a time-out is set and the time between order-select and order-sign exceeds that period, there will be no message filtering |
| Warning | FALSE | TRUE | Message filtering will be performed as normal |
| Warning | TRUE | FALSE | If a time-out is set and the time between order-select and order-sign exceeds that period, there will be no message filtering |
| Critical | FALSE | TRUE | Message filtering will be performed as normal |
| Critical | TRUE | FALSE | If a time-out is set and the time between order-select and order-sign exceeds that period, there will be no message filtering |
Since the patient ID is used to create a unique cached medication statement, if a clinician completes the order-select with patient
A but does an order-select/order-sign with patient B before completing order-sign for patient A, the message filtering
will not be affected. This may be another situation where a time-out could be beneficial for the clinician so that messages will not be filtered.
Another solution would be to track if a clinician completes order-select for a new patient before completing order-sign for their initial patient.
Clinician A completes the order-select process and clinician B completes order-sign.
| Branch triggered for both order-select and order-sign | Will alert be filtered | Description |
|---|---|---|
| Info | FALSE | Since the clinicians are different there will be no message filtering performed |
| Warning | FALSE | Since the clinicians are different there will be no message filtering performed |
| Critical | FALSE | Since the clinicians are different there will be no message filtering performed |
No cards to be filtered are returned.
The CDS Hooks specification states that the patient-view 1.0 fires when the user has just opened a patient's record.
This implementation varies from the previous Basic and Advanced as
it does not rely on medications being selected and in fact does not allow for any to be passed via the context field
of the CDS Hooks request. The context contains only the identifiers for the user and the patient, meaning that any rule
that is fired SHOULD rely on existing patient resources and prefetch data.
Figure 18 depicts the summary of operations for the Patient View Service.
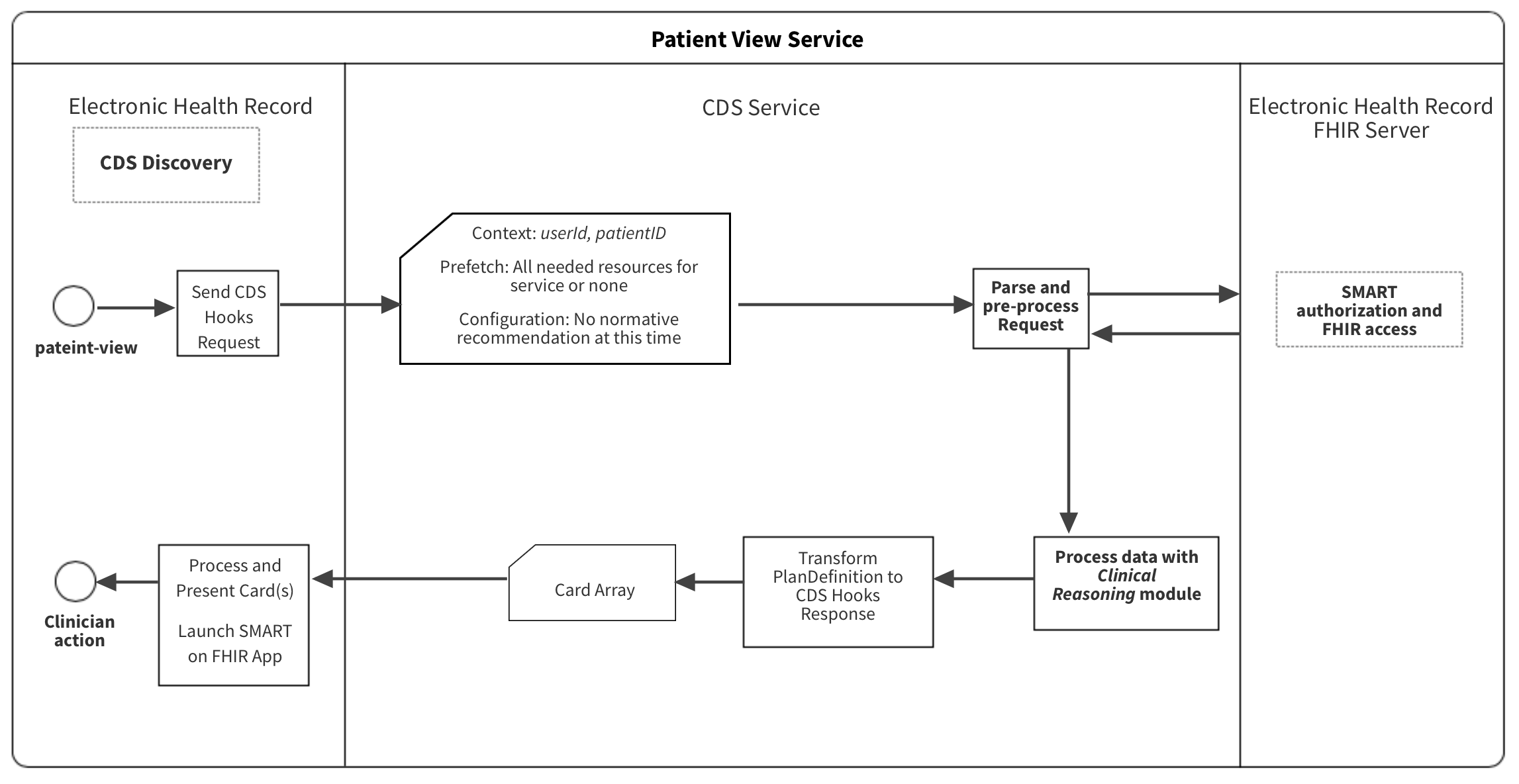
{
"services": [
{
"hook": "patient-view",
"name": "PlanDefinition - Warfarin NSAIDs Recommendation Workflow",
"title": "Warfarin NSAIDs Recommendation",
"extension": {
"configuration-items": [
{
"code": <an identifier for the configuration option>,
"type": <data type of the configuration option, e.g. boolean>,
"name": <human readable name of the configuration option>,
"description": <human readable description of the configuration option>
},
... other optional configuration options ...
]
},
"id": "warfarin-nsaids-cds-view",
"prefetch": {
"item1": "Patient?_id=",
"item2": "MedicationRequest?patient=&authoredon=ge2019-12-11",
"item3": "MedicationAdministration?patient=&effective-time=ge2019-12-11",
"item4": "MedicationDispense?patient=&whenhandedover=ge2019-12-11",
"item5": "MedicationStatement?patient=&effective=ge2019-12-11",
"item6": "Condition?patient="
}
}
]
}
Context
The context element of the patient-view CDS Hooks request differ from order-select and order-sign as there are
no selections or draftOrders. For details on the specifications are below.
patient-view 1.0
| Field | Optionality | Prefetch Token | Type | Description |
|---|---|---|---|---|
userId |
REQUIRED | Yes | string | The id of the current user. For this hook, the user is expected to be of type Practitioner. For example, Practitioner/123Describe |
patientId |
REQUIRED | Yes | string | The FHIR Patient.id of the current patient |
encounterId |
OPTIONAL | Yes | string | The FHIR Encounter.id of the current encounter |
Extension
PDDI Configuration Items
Unlike what was discussed in the Basic and Advanced
, cache-for-order-sign-filtering and filter-out-repeated-alerts serve no purpose for this request due to the timing
of when this hook is fired. Other configuration options such as alert-non-serious and show-evidence-support can be
applied here.
Prefetch
The prefetch element contains patient data that is provided by the EHR upon submission of the CDS Hook to the CDS
service. The CDS service SHOULD provide the EHR with a prefetch template at the time of service discovery. The prefetch
element MAY specify patient data other than medications for the purpose of individualizing the CDS logic and response.
The prefetch query SHOULD be designed to obtain data for the patient indicated by the context patientID.
A FHIR server request by the CDS service is necessary in the event the request prefetch element is empty. While
the prefetch element is OPTIONAL, it SHOULD NOT be partially fulfilled. The post-hoc FHIR server query is performed at
the parse and pre-process phase shown in Figure 4. To accomplish a FHIR server request, the server URL and the OAuth
authorization token (i.e. fhirServer, fhirAuthorization) SHOULD be provided in the CDS Hooks request.