CARIN Consumer Directed Payer Data Exchange (CARIN IG for Blue Button®), published by HL7 International / Financial Management. This guide is not an authorized publication; it is the continuous build for version 2.1.0 built by the FHIR (HL7® FHIR® Standard) CI Build. This version is based on the current content of https://github.com/HL7/carin-bb/ and changes regularly. See the Directory of published versions
| Page standards status: Informative |
| Term | Definition |
| Subscriber | An individual or entity that selects benefits offered by an entity, such as an employer, government, or insurance company |
| Dependent | An individual, other than the subscriber, who has insurance coverage under the benefits selected by a subscriber |
| Member | Any individual covered by the benefits offered by an entity, such as an employer or insurance company |
| Beneficiary | Any individual that selects or is covered by benefits provided by government programs |
| Patient |
An individual who has received, is receiving or intends to receive health care services. (Health care services as defined by federal and state regulations.) |
| Personal Representative | Per the HIPAA privacy regulations at 45 CFR 164.502(g), a personal-representative is someone authorized under state or other applicable law to act on behalf of the individual in making health care related decisions (such as a parent, guardian, or person with a medical power of attorney) |
| Coordination of Benefits | The process of determining which of two or more insurance policies will have the primary responsibility of processing/paying a claim and the extent to which the other policies will contribute |
| Payer |
Public or private party which offers and/or administers health insurance plan(s) or coverage and/or pays claims directly or indirectly. Examples include:
|
| Encounter data vs Claims | Encounter data means the information or data relating to the receipt of any item(s) or service(s) by an enrollee under a contract between a State and a managed care plan. Encounter data are conceptually equivalent to the paid claims records that state Medicaid agencies create when they pay providers on a FFS basis |
| EOB.careteam | The members of the team or organization who contributed to the service to the patient submitted on the claim by the billing provider to the payer |
| CareTeam Resource | The Care Team includes all the people and organizations who plan to participate in the coordination and delivery of care for a patient |
Consumer-directed exchange occurs when a consumer or an authorized caregiver invokes their HIPAA Individual Right of Access (45 CFR 164.524) and requests their digital health information from a HIPAA covered entity (CE) via an application or other third-party data steward.

 Actors:
Actors:
Flow:
The CMS Advancing Interoperability and Improving Prior Authorization Processes Proposed Rule (CMS-0057-P) requires Health Plans to adjudicated claims and encounter data (profiled in this IG available) for the Provider Access and Payer-to-Payer APIs. The data available via these APIs would be the information a Health Plan makes available to the member, with the exception that it excludes provider remittances and patient cost-sharing information.
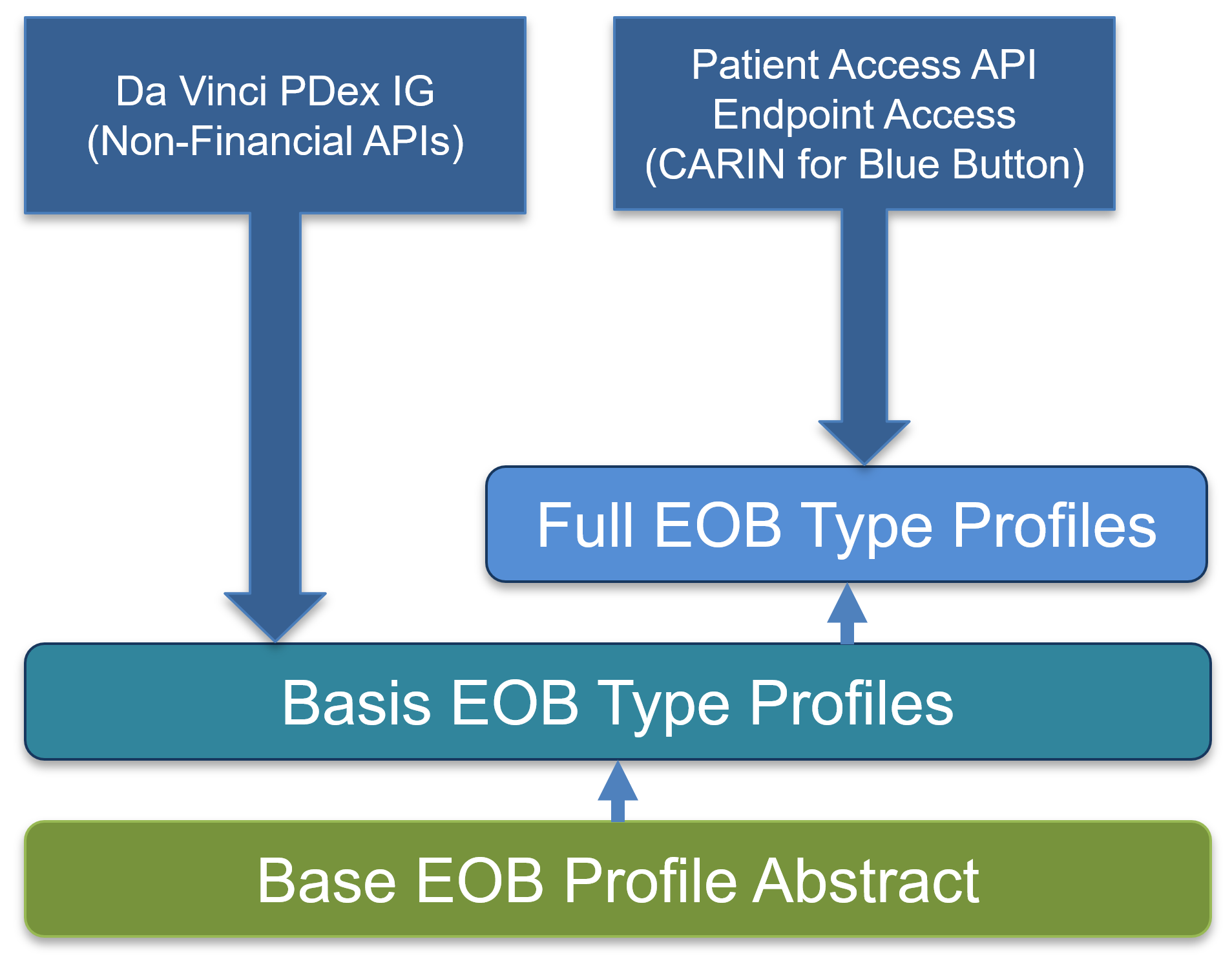
This IG addresses consumer access to claims and encounter data and does not directly address these other APIs. It does, however, contain profiles structured in a way that may used by IGs that do define the requirements of these APIs, like the Payer Data Exchange (PDex) IG, to share this information.
The below diagram shows the structure of the profiles in this IG and how they are anticipated to be used by the PDex IG where the “Basis” profiles contain all of the requirements for each type of EOB without financial data requirements and the Full EOB profiles to be used for consumer access.
</span>