PACIO Re-Assessment Timepoints Implementation Guide, published by HL7 Community-Based Care and Privacy Working Group. This is not an authorized publication; it is the continuous build for version 1.0.0). This version is based on the current content of https://github.com/HL7/fhir-pacio-rt/ and changes regularly. See the Directory of published versions
| Official URL: http://hl7.org/fhir/us/pacio-rt/StructureDefinition/reassessment-timepoints-encounter | Version: 1.0.0 | |||
| Active as of 2022-10-03 | Computable Name: ReassessmentTimepointsEncounter | |||
Re-Assessment Timepoints Encounter is a profile of the Encounter resource that allows longer-term post-acute admissions to be structured into smaller more consumable components, in line with the longer-term clinical care and progression of a patient.
Example Usage Scenarios:
Re-assessment timepoints are
The Re-Assessment Timepoints profile layers additional structure onto US Core conformant data. This structure is added to existing encounters based on regulation, payer requirements, or internal processes that result in formal assessments during post-acute care services. These formal assessments, such as the CMS Minimum Data Set (MDS) or Outcome and Assessment Information Set (OASIS), happen at the boundaries between timepoints.
The following diagram provides an overview of the existing structure (orange) and the new Re-Asssessment Timepoint structure (blue).
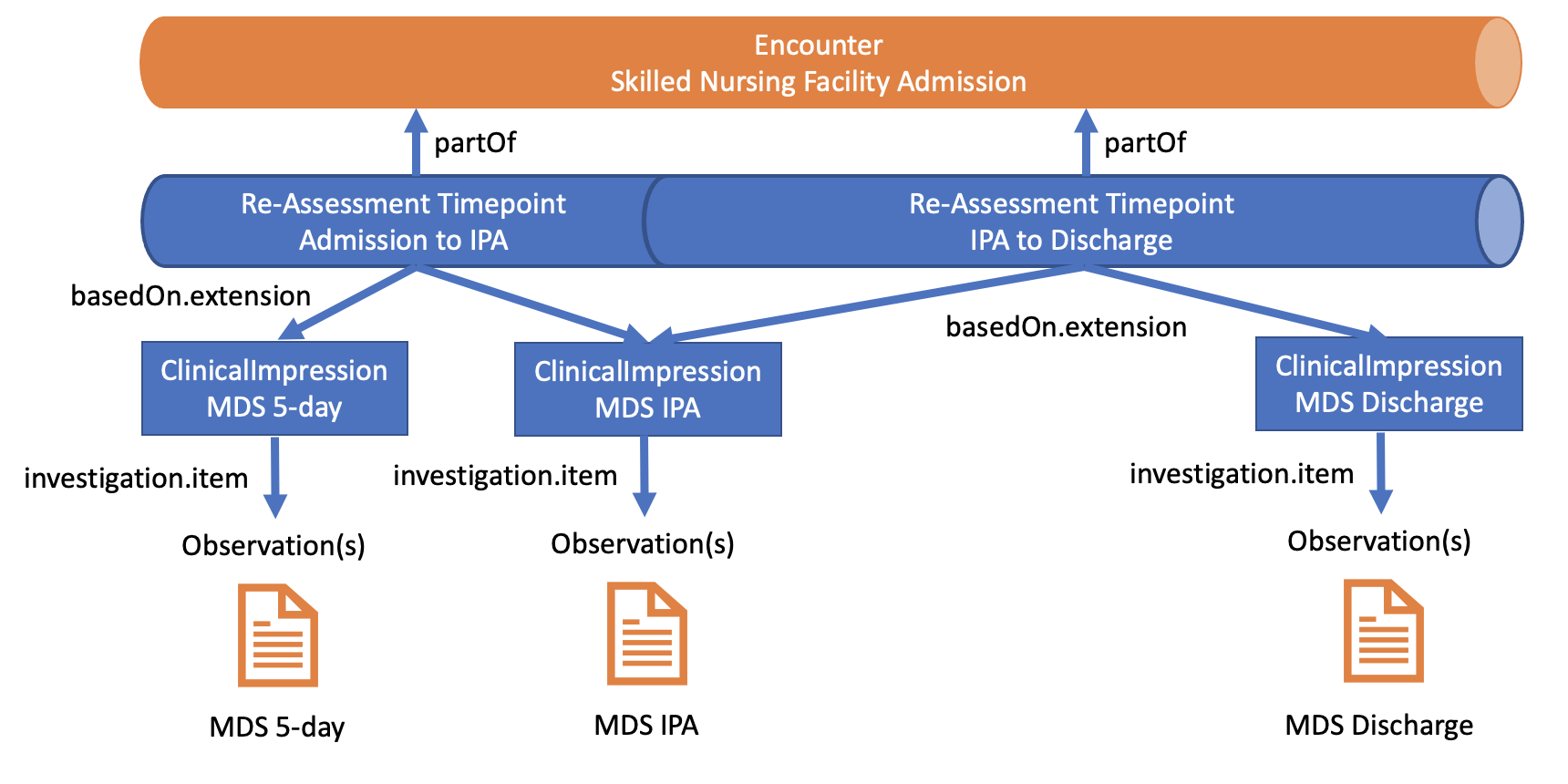
The sections below provide additional detail on these structures and their relationships.
The Re-Assessment Timepoints profile augments existing FHIR® structure for representing clinical care, specifically:
Re-Assessment Timepoint instances are created as children of the root encounter instance. Many of the associated fields duplicate the parent encounter. Specific information recorded as a part of the Re-Assessment Timepoint includes:
Clinical data SHOULD be linked explicitly to the Re-Assessment Timepoint Encounter through associated ClinicalImpression instances. This IG does not profile ClinicalImpression, so the intended use of the structure is described here. Each ClinicalImpression instance represents a formal assessment, such as the MDS 5-day or OASIS 120-day Follow-up. An entry in the investigation field lists references to the Observation instances that document these assessments in investigation.item.
ClinicalImpression instances are linked to relevant Re-Assessment Timepoints via the basedOn extension within the timepoint instance itself. ClinicalImpression instances will be linked in this way to the Re-Assessment Timepoint that the associated assessment initiates, the Re-Assessment Timepoint that the associated assessment concludes, or both.
The following data elements must always be present or must be supported if the data is present in the sending system (Must Support definition). They are presented below with a simple human-readable explanation. Profile specific guidance and examples are provided as well. The Formal Profile Definition below provides the formal summary, definitions, and terminology requirements.
Each Re-Assessment Timepoint Encounter must have:
Each Re-Assessment Timepoint Encounter must support:
Usage:
Description of Profiles, Differentials, Snapshots and how the different presentations work.
This structure is derived from USCoreEncounterProfile
Summary
Mandatory: 8 elements
Must-Support: 8 elements
Structures
This structure refers to these other structures:
Extensions
This structure refers to these extensions:
This structure is derived from USCoreEncounterProfile
| Name | Flags | Card. | Type | Description & Constraints |
|---|---|---|---|---|
 | 0..* | USCoreEncounterProfile | An interaction during which services are provided to the patient | |
  | 1..* | Identifier | Identifier(s) by which this timepoint is known | |
  | 1..1 | code | in-progress | finished | planned Binding: Timepoint Status Value Set (required) | |
  | S | 0..* | BackboneElement | List of past timepoint statuses |
   | 1..1 | code | in-progress | finished | planned Binding: Timepoint Status Value Set (required) | |
  | 1..1 | Coding | Classification of patient timepoint Binding: Timepoint Class Value Set (extensible) | |
  | 0..* | BackboneElement | List of past timepoint classes | |
   | 1..1 | Coding | inpatient | outpatient | ambulatory | emergency + Binding: Timepoint Class Value Set (extensible) | |
  | 1..* | CodeableConcept | The entity structuring the timepoint Binding: Timepoint Entity Type Value Set (extensible) | |
  | S | 1..1 | CodeableConcept | The assessment or instrument driving the timepoint Binding: Timepoint Service Type Value Set (extensible) |
  | 0..1 | CodeableConcept | Indicates the urgency of the timepoint | |
  | 1..1 | Reference(US Core Patient Profile) | The patient present at the timepoint | |
  | S | 0..* | Reference(EpisodeOfCare) | Episode(s) of care that this timepoint should be recorded against |
  | ||||
   | S | 0..* | Reference(ClinicalImpression) | Clinical Impression can reflect any and all clinical related data tied to the assessment/instrument driving the timepoint, or within the timepoint itself. URL: http://hl7.org/fhir/us/pacio-rt/StructureDefinition/clinicalImpression |
  | 1..* | BackboneElement | Clinicians or Care Teams active in a timepoint | |
   | 0..* | CodeableConcept | Role of participant in timepoint | |
   | 0..1 | Period | Period of time during the timepoint that the participant participated | |
   | 0..1 | Reference(US Core Practitioner Profile) | Persons involved in the timepoint other than the patient | |
  | 0..* | Reference(Appointment) | Scheduled appointment or appointments that start the timepoint. | |
  | 1..1 | Period | The start and end date/time of the timepoint | |
  | 0..1 | Duration | Days in a given timepoint period. | |
  | 1..* | CodeableConcept | The ICD or Snomed Code that is the subject of the given timepoint | |
  | S | 0..* | Reference(US Core Condition Profile | US Core Procedure Profile | Observation) | Reason the timepoint takes place (reference) |
  | S | 0..* | BackboneElement | Holding all DX codes for given patient during a given timepoint. |
   | 1..1 | Reference(Condition | Procedure) | The diagnosis or procedure relevant to the timepoint | |
   | 0..1 | CodeableConcept | Role that this diagnosis has within the timepoint (e.g. admission, billing, discharge …) | |
  | 0..* | Reference(Account) | The set of accounts that may be used for billing for this timepoint. | |
  | 1..* | BackboneElement | List of locations where the patient has been during this timepoint. | |
   | 1..1 | Reference(US Core Location Profile) | The location where the timepoint takes place. | |
  | S | 1..1 | Reference(US Core Organization Profile) | The organization (facility) responsible for this timepoint |
  | S | 1..1 | Reference(US Core Encounter Profile) | The Encounter this timepoint is part of |
 Documentation for this format Documentation for this format | ||||
| Name | Flags | Card. | Type | Description & Constraints | ||||
|---|---|---|---|---|---|---|---|---|
 | 0..* | USCoreEncounterProfile | An interaction during which services are provided to the patient | |||||
  | Σ | 0..1 | id | Logical id of this artifact | ||||
  | Σ | 0..1 | Meta | Metadata about the resource | ||||
  | ?!Σ | 0..1 | uri | A set of rules under which this content was created | ||||
  | 0..1 | code | Language of the resource content Binding: CommonLanguages (preferred): A human language.
| |||||
  | 0..1 | Narrative | Text summary of the resource, for human interpretation | |||||
  | 0..* | Resource | Contained, inline Resources | |||||
  | 0..* | Extension | Additional content defined by implementations | |||||
  | ?! | 0..* | Extension | Extensions that cannot be ignored | ||||
  | SΣ | 1..* | Identifier | Identifier(s) by which this timepoint is known | ||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   | ?!Σ | 0..1 | code | usual | official | temp | secondary | old (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
   | Σ | 0..1 | CodeableConcept | Description of identifier Binding: Identifier Type Codes (extensible): A coded type for an identifier that can be used to determine which identifier to use for a specific purpose. | ||||
   | SΣ | 1..1 | uri | The namespace for the identifier value Example General: http://www.acme.com/identifiers/patient | ||||
   | SΣ | 1..1 | string | The value that is unique Example General: 123456 | ||||
   | Σ | 0..1 | Period | Time period when id is/was valid for use | ||||
   | Σ | 0..1 | Reference(Organization) | Organization that issued id (may be just text) | ||||
  | ?!SΣ | 1..1 | code | in-progress | finished | planned Binding: Timepoint Status Value Set (required) | ||||
  | S | 0..* | BackboneElement | List of past timepoint statuses | ||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   | 1..1 | code | in-progress | finished | planned Binding: Timepoint Status Value Set (required) | |||||
   | 1..1 | Period | The time that the episode was in the specified status | |||||
  | SΣ | 1..1 | Coding | Classification of patient timepoint Binding: Timepoint Class Value Set (extensible) | ||||
  | 0..* | BackboneElement | List of past timepoint classes | |||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   | 1..1 | Coding | inpatient | outpatient | ambulatory | emergency + Binding: Timepoint Class Value Set (extensible) | |||||
   | 1..1 | Period | The time that the episode was in the specified class | |||||
  | SΣ | 1..* | CodeableConcept | The entity structuring the timepoint Binding: Timepoint Entity Type Value Set (extensible) | ||||
  | SΣ | 1..1 | CodeableConcept | The assessment or instrument driving the timepoint Binding: Timepoint Service Type Value Set (extensible) | ||||
  | 0..1 | CodeableConcept | Indicates the urgency of the timepoint Binding: ActPriority (example): Indicates the urgency of the encounter. | |||||
  | SΣ | 1..1 | Reference(US Core Patient Profile) | The patient present at the timepoint | ||||
  | SΣ | 0..* | Reference(EpisodeOfCare) | Episode(s) of care that this timepoint should be recorded against | ||||
  | 0..* | Reference(ServiceRequest) | The ServiceRequest that initiated this encounter | |||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   | S | 0..* | Reference(ClinicalImpression) | Clinical Impression can reflect any and all clinical related data tied to the assessment/instrument driving the timepoint, or within the timepoint itself. URL: http://hl7.org/fhir/us/pacio-rt/StructureDefinition/clinicalImpression | ||||
   | ΣC | 0..1 | string | Literal reference, Relative, internal or absolute URL | ||||
   | Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
   | Σ | 0..1 | Identifier | Logical reference, when literal reference is not known | ||||
   | Σ | 0..1 | string | Text alternative for the resource | ||||
  | SΣ | 1..* | BackboneElement | Clinicians or Care Teams active in a timepoint | ||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   | SΣ | 0..* | CodeableConcept | Role of participant in timepoint Binding: ParticipantType (extensible): Role of participant in encounter. | ||||
   | S | 0..1 | Period | Period of time during the timepoint that the participant participated | ||||
   | SΣ | 0..1 | Reference(US Core Practitioner Profile) | Persons involved in the timepoint other than the patient | ||||
  | Σ | 0..* | Reference(Appointment) | Scheduled appointment or appointments that start the timepoint. | ||||
  | S | 1..1 | Period | The start and end date/time of the timepoint | ||||
  | 0..1 | Duration | Days in a given timepoint period. | |||||
  | SΣ | 1..* | CodeableConcept | The ICD or Snomed Code that is the subject of the given timepoint Binding: EncounterReasonCodes (preferred): Reason why the encounter takes place. | ||||
  | SΣ | 0..* | Reference(US Core Condition Profile | US Core Procedure Profile | Observation) | Reason the timepoint takes place (reference) | ||||
  | SΣ | 0..* | BackboneElement | Holding all DX codes for given patient during a given timepoint. | ||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   | Σ | 1..1 | Reference(Condition | Procedure) | The diagnosis or procedure relevant to the timepoint | ||||
   | 0..1 | CodeableConcept | Role that this diagnosis has within the timepoint (e.g. admission, billing, discharge …) Binding: DiagnosisRole (preferred): The type of diagnosis this condition represents. | |||||
   | 0..1 | positiveInt | Ranking of the diagnosis (for each role type) | |||||
  | 0..* | Reference(Account) | The set of accounts that may be used for billing for this timepoint. | |||||
  | S | 0..1 | BackboneElement | Details about the admission to a healthcare service | ||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   | 0..1 | Identifier | Pre-admission identifier | |||||
   | 0..1 | Reference(Location | Organization) | The location/organization from which the patient came before admission | |||||
   | 0..1 | CodeableConcept | From where patient was admitted (physician referral, transfer) Binding: AdmitSource (preferred): From where the patient was admitted. | |||||
   | 0..1 | CodeableConcept | The type of hospital re-admission that has occurred (if any). If the value is absent, then this is not identified as a readmission Binding: hl7VS-re-admissionIndicator (example): The reason for re-admission of this hospitalization encounter. | |||||
   | 0..* | CodeableConcept | Diet preferences reported by the patient Binding: Diet (example): Medical, cultural or ethical food preferences to help with catering requirements. | |||||
   | 0..* | CodeableConcept | Special courtesies (VIP, board member) Binding: SpecialCourtesy (preferred): Special courtesies. | |||||
   | 0..* | CodeableConcept | Wheelchair, translator, stretcher, etc. Binding: SpecialArrangements (preferred): Special arrangements. | |||||
   | 0..1 | Reference(Location | Organization) | Location/organization to which the patient is discharged | |||||
   | S | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: DischargeDisposition (example): Discharge Disposition. | ||||
  | S | 1..* | BackboneElement | List of locations where the patient has been during this timepoint. | ||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   | S | 1..1 | Reference(US Core Location Profile) | The location where the timepoint takes place. | ||||
   | 0..1 | code | planned | active | reserved | completed Binding: EncounterLocationStatus (required): The status of the location. | |||||
   | 0..1 | CodeableConcept | The physical type of the location (usually the level in the location hierachy - bed room ward etc.) Binding: LocationType (example): Physical form of the location. | |||||
   | 0..1 | Period | Time period during which the patient was present at the location | |||||
  | S | 1..1 | Reference(US Core Organization Profile) | The organization (facility) responsible for this timepoint | ||||
  | S | 1..1 | Reference(US Core Encounter Profile) | The Encounter this timepoint is part of | ||||
 Documentation for this format Documentation for this format | ||||||||
| Name | Flags | Card. | Type | Description & Constraints |
|---|---|---|---|---|
 | 0..* | USCoreEncounterProfile | An interaction during which services are provided to the patient | |
  | Σ | 1..* | Identifier | Identifier(s) by which this timepoint is known |
   | Σ | 1..1 | uri | The namespace for the identifier value |
   | Σ | 1..1 | string | The value that is unique |
  | ?!Σ | 1..1 | code | in-progress | finished | planned Binding: Timepoint Status Value Set (required) |
  | 0..* | BackboneElement | List of past timepoint statuses | |
  | Σ | 1..1 | Coding | Classification of patient timepoint Binding: Timepoint Class Value Set (extensible) |
  | Σ | 1..* | CodeableConcept | The entity structuring the timepoint Binding: Timepoint Entity Type Value Set (extensible) |
  | Σ | 1..1 | CodeableConcept | The assessment or instrument driving the timepoint Binding: Timepoint Service Type Value Set (extensible) |
  | Σ | 1..1 | Reference(US Core Patient Profile) | The patient present at the timepoint |
  | Σ | 0..* | Reference(EpisodeOfCare) | Episode(s) of care that this timepoint should be recorded against |
  | 0..* | Reference(ServiceRequest) | The ServiceRequest that initiated this encounter | |
   | 0..* | Reference(ClinicalImpression) | Clinical Impression can reflect any and all clinical related data tied to the assessment/instrument driving the timepoint, or within the timepoint itself. URL: http://hl7.org/fhir/us/pacio-rt/StructureDefinition/clinicalImpression | |
  | Σ | 1..* | BackboneElement | Clinicians or Care Teams active in a timepoint |
   | Σ | 0..* | CodeableConcept | Role of participant in timepoint Binding: ParticipantType (extensible): Role of participant in encounter. |
   | 0..1 | Period | Period of time during the timepoint that the participant participated | |
   | Σ | 0..1 | Reference(US Core Practitioner Profile) | Persons involved in the timepoint other than the patient |
  | 1..1 | Period | The start and end date/time of the timepoint | |
  | Σ | 1..* | CodeableConcept | The ICD or Snomed Code that is the subject of the given timepoint Binding: EncounterReasonCodes (preferred): Reason why the encounter takes place. |
  | Σ | 0..* | Reference(US Core Condition Profile | US Core Procedure Profile | Observation) | Reason the timepoint takes place (reference) |
  | Σ | 0..* | BackboneElement | Holding all DX codes for given patient during a given timepoint. |
  | 0..1 | BackboneElement | Details about the admission to a healthcare service | |
   | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: DischargeDisposition (example): Discharge Disposition. | |
  | 1..* | BackboneElement | List of locations where the patient has been during this timepoint. | |
   | 1..1 | Reference(US Core Location Profile) | The location where the timepoint takes place. | |
  | 1..1 | Reference(US Core Organization Profile) | The organization (facility) responsible for this timepoint | |
  | 1..1 | Reference(US Core Encounter Profile) | The Encounter this timepoint is part of | |
 Documentation for this format Documentation for this format | ||||
This structure is derived from USCoreEncounterProfile
Summary
Mandatory: 8 elements
Must-Support: 8 elements
Structures
This structure refers to these other structures:
Extensions
This structure refers to these extensions:
Differential View
This structure is derived from USCoreEncounterProfile
| Name | Flags | Card. | Type | Description & Constraints |
|---|---|---|---|---|
 | 0..* | USCoreEncounterProfile | An interaction during which services are provided to the patient | |
  | 1..* | Identifier | Identifier(s) by which this timepoint is known | |
  | 1..1 | code | in-progress | finished | planned Binding: Timepoint Status Value Set (required) | |
  | S | 0..* | BackboneElement | List of past timepoint statuses |
   | 1..1 | code | in-progress | finished | planned Binding: Timepoint Status Value Set (required) | |
  | 1..1 | Coding | Classification of patient timepoint Binding: Timepoint Class Value Set (extensible) | |
  | 0..* | BackboneElement | List of past timepoint classes | |
   | 1..1 | Coding | inpatient | outpatient | ambulatory | emergency + Binding: Timepoint Class Value Set (extensible) | |
  | 1..* | CodeableConcept | The entity structuring the timepoint Binding: Timepoint Entity Type Value Set (extensible) | |
  | S | 1..1 | CodeableConcept | The assessment or instrument driving the timepoint Binding: Timepoint Service Type Value Set (extensible) |
  | 0..1 | CodeableConcept | Indicates the urgency of the timepoint | |
  | 1..1 | Reference(US Core Patient Profile) | The patient present at the timepoint | |
  | S | 0..* | Reference(EpisodeOfCare) | Episode(s) of care that this timepoint should be recorded against |
  | ||||
   | S | 0..* | Reference(ClinicalImpression) | Clinical Impression can reflect any and all clinical related data tied to the assessment/instrument driving the timepoint, or within the timepoint itself. URL: http://hl7.org/fhir/us/pacio-rt/StructureDefinition/clinicalImpression |
  | 1..* | BackboneElement | Clinicians or Care Teams active in a timepoint | |
   | 0..* | CodeableConcept | Role of participant in timepoint | |
   | 0..1 | Period | Period of time during the timepoint that the participant participated | |
   | 0..1 | Reference(US Core Practitioner Profile) | Persons involved in the timepoint other than the patient | |
  | 0..* | Reference(Appointment) | Scheduled appointment or appointments that start the timepoint. | |
  | 1..1 | Period | The start and end date/time of the timepoint | |
  | 0..1 | Duration | Days in a given timepoint period. | |
  | 1..* | CodeableConcept | The ICD or Snomed Code that is the subject of the given timepoint | |
  | S | 0..* | Reference(US Core Condition Profile | US Core Procedure Profile | Observation) | Reason the timepoint takes place (reference) |
  | S | 0..* | BackboneElement | Holding all DX codes for given patient during a given timepoint. |
   | 1..1 | Reference(Condition | Procedure) | The diagnosis or procedure relevant to the timepoint | |
   | 0..1 | CodeableConcept | Role that this diagnosis has within the timepoint (e.g. admission, billing, discharge …) | |
  | 0..* | Reference(Account) | The set of accounts that may be used for billing for this timepoint. | |
  | 1..* | BackboneElement | List of locations where the patient has been during this timepoint. | |
   | 1..1 | Reference(US Core Location Profile) | The location where the timepoint takes place. | |
  | S | 1..1 | Reference(US Core Organization Profile) | The organization (facility) responsible for this timepoint |
  | S | 1..1 | Reference(US Core Encounter Profile) | The Encounter this timepoint is part of |
 Documentation for this format Documentation for this format | ||||
Snapshot View
| Name | Flags | Card. | Type | Description & Constraints | ||||
|---|---|---|---|---|---|---|---|---|
 | 0..* | USCoreEncounterProfile | An interaction during which services are provided to the patient | |||||
  | Σ | 0..1 | id | Logical id of this artifact | ||||
  | Σ | 0..1 | Meta | Metadata about the resource | ||||
  | ?!Σ | 0..1 | uri | A set of rules under which this content was created | ||||
  | 0..1 | code | Language of the resource content Binding: CommonLanguages (preferred): A human language.
| |||||
  | 0..1 | Narrative | Text summary of the resource, for human interpretation | |||||
  | 0..* | Resource | Contained, inline Resources | |||||
  | 0..* | Extension | Additional content defined by implementations | |||||
  | ?! | 0..* | Extension | Extensions that cannot be ignored | ||||
  | SΣ | 1..* | Identifier | Identifier(s) by which this timepoint is known | ||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   | ?!Σ | 0..1 | code | usual | official | temp | secondary | old (If known) Binding: IdentifierUse (required): Identifies the purpose for this identifier, if known . | ||||
   | Σ | 0..1 | CodeableConcept | Description of identifier Binding: Identifier Type Codes (extensible): A coded type for an identifier that can be used to determine which identifier to use for a specific purpose. | ||||
   | SΣ | 1..1 | uri | The namespace for the identifier value Example General: http://www.acme.com/identifiers/patient | ||||
   | SΣ | 1..1 | string | The value that is unique Example General: 123456 | ||||
   | Σ | 0..1 | Period | Time period when id is/was valid for use | ||||
   | Σ | 0..1 | Reference(Organization) | Organization that issued id (may be just text) | ||||
  | ?!SΣ | 1..1 | code | in-progress | finished | planned Binding: Timepoint Status Value Set (required) | ||||
  | S | 0..* | BackboneElement | List of past timepoint statuses | ||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   | 1..1 | code | in-progress | finished | planned Binding: Timepoint Status Value Set (required) | |||||
   | 1..1 | Period | The time that the episode was in the specified status | |||||
  | SΣ | 1..1 | Coding | Classification of patient timepoint Binding: Timepoint Class Value Set (extensible) | ||||
  | 0..* | BackboneElement | List of past timepoint classes | |||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   | 1..1 | Coding | inpatient | outpatient | ambulatory | emergency + Binding: Timepoint Class Value Set (extensible) | |||||
   | 1..1 | Period | The time that the episode was in the specified class | |||||
  | SΣ | 1..* | CodeableConcept | The entity structuring the timepoint Binding: Timepoint Entity Type Value Set (extensible) | ||||
  | SΣ | 1..1 | CodeableConcept | The assessment or instrument driving the timepoint Binding: Timepoint Service Type Value Set (extensible) | ||||
  | 0..1 | CodeableConcept | Indicates the urgency of the timepoint Binding: ActPriority (example): Indicates the urgency of the encounter. | |||||
  | SΣ | 1..1 | Reference(US Core Patient Profile) | The patient present at the timepoint | ||||
  | SΣ | 0..* | Reference(EpisodeOfCare) | Episode(s) of care that this timepoint should be recorded against | ||||
  | 0..* | Reference(ServiceRequest) | The ServiceRequest that initiated this encounter | |||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations Slice: Unordered, Open by value:url | |||||
   | S | 0..* | Reference(ClinicalImpression) | Clinical Impression can reflect any and all clinical related data tied to the assessment/instrument driving the timepoint, or within the timepoint itself. URL: http://hl7.org/fhir/us/pacio-rt/StructureDefinition/clinicalImpression | ||||
   | ΣC | 0..1 | string | Literal reference, Relative, internal or absolute URL | ||||
   | Σ | 0..1 | uri | Type the reference refers to (e.g. "Patient") Binding: ResourceType (extensible): Aa resource (or, for logical models, the URI of the logical model). | ||||
   | Σ | 0..1 | Identifier | Logical reference, when literal reference is not known | ||||
   | Σ | 0..1 | string | Text alternative for the resource | ||||
  | SΣ | 1..* | BackboneElement | Clinicians or Care Teams active in a timepoint | ||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   | SΣ | 0..* | CodeableConcept | Role of participant in timepoint Binding: ParticipantType (extensible): Role of participant in encounter. | ||||
   | S | 0..1 | Period | Period of time during the timepoint that the participant participated | ||||
   | SΣ | 0..1 | Reference(US Core Practitioner Profile) | Persons involved in the timepoint other than the patient | ||||
  | Σ | 0..* | Reference(Appointment) | Scheduled appointment or appointments that start the timepoint. | ||||
  | S | 1..1 | Period | The start and end date/time of the timepoint | ||||
  | 0..1 | Duration | Days in a given timepoint period. | |||||
  | SΣ | 1..* | CodeableConcept | The ICD or Snomed Code that is the subject of the given timepoint Binding: EncounterReasonCodes (preferred): Reason why the encounter takes place. | ||||
  | SΣ | 0..* | Reference(US Core Condition Profile | US Core Procedure Profile | Observation) | Reason the timepoint takes place (reference) | ||||
  | SΣ | 0..* | BackboneElement | Holding all DX codes for given patient during a given timepoint. | ||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   | Σ | 1..1 | Reference(Condition | Procedure) | The diagnosis or procedure relevant to the timepoint | ||||
   | 0..1 | CodeableConcept | Role that this diagnosis has within the timepoint (e.g. admission, billing, discharge …) Binding: DiagnosisRole (preferred): The type of diagnosis this condition represents. | |||||
   | 0..1 | positiveInt | Ranking of the diagnosis (for each role type) | |||||
  | 0..* | Reference(Account) | The set of accounts that may be used for billing for this timepoint. | |||||
  | S | 0..1 | BackboneElement | Details about the admission to a healthcare service | ||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   | 0..1 | Identifier | Pre-admission identifier | |||||
   | 0..1 | Reference(Location | Organization) | The location/organization from which the patient came before admission | |||||
   | 0..1 | CodeableConcept | From where patient was admitted (physician referral, transfer) Binding: AdmitSource (preferred): From where the patient was admitted. | |||||
   | 0..1 | CodeableConcept | The type of hospital re-admission that has occurred (if any). If the value is absent, then this is not identified as a readmission Binding: hl7VS-re-admissionIndicator (example): The reason for re-admission of this hospitalization encounter. | |||||
   | 0..* | CodeableConcept | Diet preferences reported by the patient Binding: Diet (example): Medical, cultural or ethical food preferences to help with catering requirements. | |||||
   | 0..* | CodeableConcept | Special courtesies (VIP, board member) Binding: SpecialCourtesy (preferred): Special courtesies. | |||||
   | 0..* | CodeableConcept | Wheelchair, translator, stretcher, etc. Binding: SpecialArrangements (preferred): Special arrangements. | |||||
   | 0..1 | Reference(Location | Organization) | Location/organization to which the patient is discharged | |||||
   | S | 0..1 | CodeableConcept | Category or kind of location after discharge Binding: DischargeDisposition (example): Discharge Disposition. | ||||
  | S | 1..* | BackboneElement | List of locations where the patient has been during this timepoint. | ||||
   | 0..1 | string | Unique id for inter-element referencing | |||||
   | 0..* | Extension | Additional content defined by implementations | |||||
   | ?!Σ | 0..* | Extension | Extensions that cannot be ignored even if unrecognized | ||||
   | S | 1..1 | Reference(US Core Location Profile) | The location where the timepoint takes place. | ||||
   | 0..1 | code | planned | active | reserved | completed Binding: EncounterLocationStatus (required): The status of the location. | |||||
   | 0..1 | CodeableConcept | The physical type of the location (usually the level in the location hierachy - bed room ward etc.) Binding: LocationType (example): Physical form of the location. | |||||
   | 0..1 | Period | Time period during which the patient was present at the location | |||||
  | S | 1..1 | Reference(US Core Organization Profile) | The organization (facility) responsible for this timepoint | ||||
  | S | 1..1 | Reference(US Core Encounter Profile) | The Encounter this timepoint is part of | ||||
 Documentation for this format Documentation for this format | ||||||||
Other representations of profile: CSV, Excel, Schematron
| Path | Conformance | ValueSet |
| Encounter.language | preferred | CommonLanguages Max Binding: AllLanguages |
| Encounter.identifier.use | required | IdentifierUse |
| Encounter.identifier.type | extensible | Identifier Type Codes |
| Encounter.status | required | TimepointStatusValueSet |
| Encounter.statusHistory.status | required | TimepointStatusValueSet |
| Encounter.class | extensible | TimepointClassValueSet |
| Encounter.classHistory.class | extensible | TimepointClassValueSet |
| Encounter.type | extensible | TimepointEntityTypeValueSet (a valid code from Timepoint Entity Code System) |
| Encounter.serviceType | extensible | TimepointServiceTypeValueSet (a valid code from Timepoint Service Type Code System) |
| Encounter.priority | example | ActPriority |
| Encounter.basedOn.type | extensible | ResourceType |
| Encounter.participant.type | extensible | ParticipantType |
| Encounter.reasonCode | preferred | EncounterReasonCodes |
| Encounter.diagnosis.use | preferred | DiagnosisRole |
| Encounter.hospitalization.admitSource | preferred | AdmitSource |
| Encounter.hospitalization.reAdmission | example | Hl7VSReAdmissionIndicator |
| Encounter.hospitalization.dietPreference | example | Diet |
| Encounter.hospitalization.specialCourtesy | preferred | SpecialCourtesy |
| Encounter.hospitalization.specialArrangement | preferred | SpecialArrangements |
| Encounter.hospitalization.dischargeDisposition | example | DischargeDisposition |
| Encounter.location.status | required | EncounterLocationStatus |
| Encounter.location.physicalType | example | LocationType |
The following search parameters and search parameter combinations SHALL be supported:
SHALL support searching for all encounters, including re-assessment timepoints, that are children of another encounter using the part-of search parameter:
GET [base]/Encounter?part-of={Type/}[id]
Example:
Implementation Notes: Fetches a bundle of all Encounter resources, including Re-Assessment Timepoint Encounter resources, that are children of the specified encounter (how to search by reference)
part-of and date search parameters:
date comparators: gt,lt,ge,ledate (e.g.date=[date]&date=[date]]&...)GET [base]/Encounter?date={gt|lt|ge|le}[date]{&date={gt|lt|ge|le}[date]&...}&part-of={Type/}[id]
Example:
Implementation Notes: Fetches a bundle of all Encounter resources, including Re-Assessment Timepoint Encounter resources, matching the specified date and parent Encounter (how to search by date and how to search by reference)
SHALL support searching for all encounters, including re-assessment timepoint encounters, for a patient using the patient search parameter:
GET [base]/Encounter?patient={Type/}[id]
Example:
Implementation Notes: Fetches a bundle of all Encounter resources, including Re-Assessment Timepoint Encounter resources, for the specified patient ([how to search by reference])
patient and date search parameters:
date comparators: gt,lt,ge,ledate (e.g.date=[date]&date=[date]]&...)GET [base]/Encounter?date={gt|lt|ge|le}[date]{&date={gt|lt|ge|le}[date]&...}&patient={Type/}[id]
Example:
Implementation Notes: Fetches a bundle of all Encounter resources, including Re-Assessment Timepoint Encounter resources, matching the specified date and patient (how to search by date and how to search by reference)
SHALL support fetching a re-assessment timepoint using the _id search parameter:
GET [base]/Encounter[id]
Example:
Implementation Notes: Fetches a single Re-Assessment Timepoint Encounter resource (how to search by the logical id of the resource)
date and patient search parameters:
date comparators: gt,lt,ge,ledate (e.g.date=[date]&date=[date]]&...)GET [base]/Encounter?date={gt|lt|ge|le}[date]{&date={gt|lt|ge|le}[date]&...}&patient={Type/}[id]
Example:
Implementation Notes: Fetches a bundle of all Encounter resources, including Re-Assessment Timepoint Encounter resources, matching the specified date and patient (how to search by date and how to search by reference)
date search parameter:
date comparators: gt,lt,ge,ledate (e.g.date=[date]&date=[date]]&...)GET [base]/Encounter?date={gt|lt|ge|le}[date]{&date={gt|lt|ge|le}[date]&...}
Example:
Implementation Notes: Fetches a bundle of all Encounter resources, including Re-Assessment Timepoints, matching the specified date (how to search by date)
SHALL support searching for all encounters, including re-assessment timepoints, using the episode-of-care search parameter:
GET [base]/Encounter?episode-of-care={Type/}[id]
Example:
Implementation Notes: Fetches a bundle of all Encounter resources, including Re-Assessment Timepoint Encounter resources, that are children of the episode of care (how to search by reference)
The following search parameters SHOULD be supported. In addition, search parameters which are supported individually SHOULD also be supported in combination with any set of other individually supported search parameters.
SHOULD support searching for all encounters, including re-assessment timepoints, using the based-on search parameter:
GET [base]/Encounter?based-on={Type/}[id]
Example:
Implementation Notes: Fetches a bundle containing any Encounter resources, including Re-Assessment Timepoint Encounter resources, referencing the ClinicalImpression or ServiceRequest instance (how to search by reference)
SHOULD support searching for all encounters, including re-assessment timepoints, using the diagnosis search parameter:
GET [base]/Encounter?diagnosis={Type/}[id]
Example:
Implementation Notes: Fetches a bundle containing any Encounter resources, including Re-Assessment Timepoint Encounter resources, referencing the Condition or Procedure instance (how to search by reference)
SHOULD support searching for all encounters, including re-assessment timepoints, using the reason-reference search parameter:
GET [base]/Encounter?reason-reference={Type/}[id]
Example:
Implementation Notes: Fetches a bundle containing any Encounter resources, including Re-Assessment Timepoint Encounter resources, referencing the Condition, Procedure, or Observation instance (how to search by reference)
SHOULD support searching for all encounters, including re-assessment timepoints, using the service-provider search parameter:
GET [base]/Encounter?service-provider={Type/}[id]
Example:
Implementation Notes: Fetches a bundle containing any Encounter resources, including Re-Assessment Timepoint Encounter resources, referencing the Organization instance (how to search by reference)
SHOULD support searching for all encounters, including re-assessment timepoints, using the status search parameter:
GET [base]/Encounter?status={Type/}[id]
Example:
Implementation Notes: Fetches a bundle containing any Encounter resources, including Re-Assessment Timepoint Encounter resources, matching the status (how to search by token)