PACIO Re-Assessment Timepoints Implementation Guide, published by HL7 Community-Based Care and Privacy Working Group. This is not an authorized publication; it is the continuous build for version 1.0.0). This version is based on the current content of https://github.com/HL7/fhir-pacio-rt/ and changes regularly. See the Directory of published versions
| Official URL: http://hl7.org/fhir/us/pacio-rt/ImplementationGuide/hl7.fhir.us.pacio-rt | Version: 1.0.0 | |||
| Active as of 2022-10-03 | Computable Name: PACIOReAssessmentTimepoints | |||
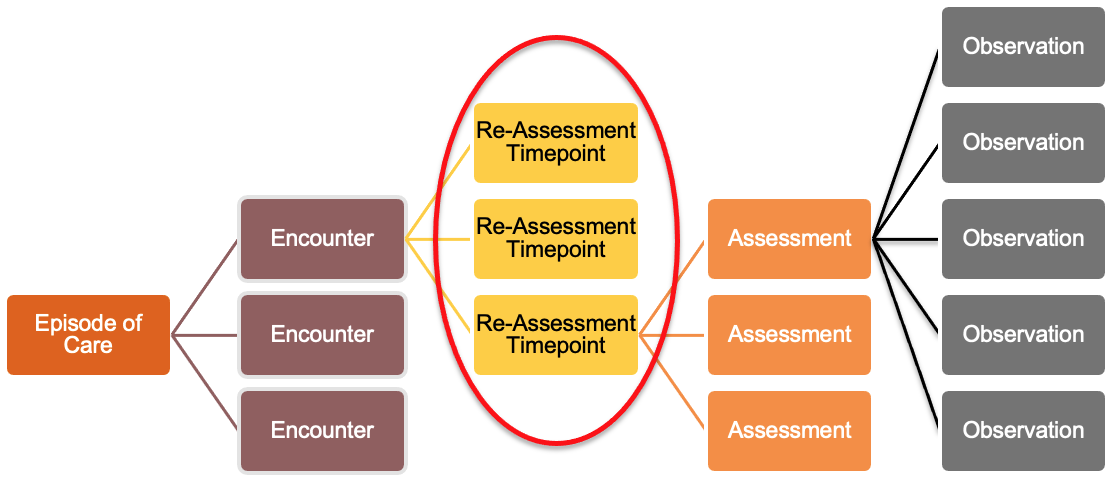
The Re-Assessment Timepoints implementation guide (IG) describes a means to break up extended Post-Acute admissions into consumable blocks that can reflect the evolution of care over time of the encounter or episode of care.
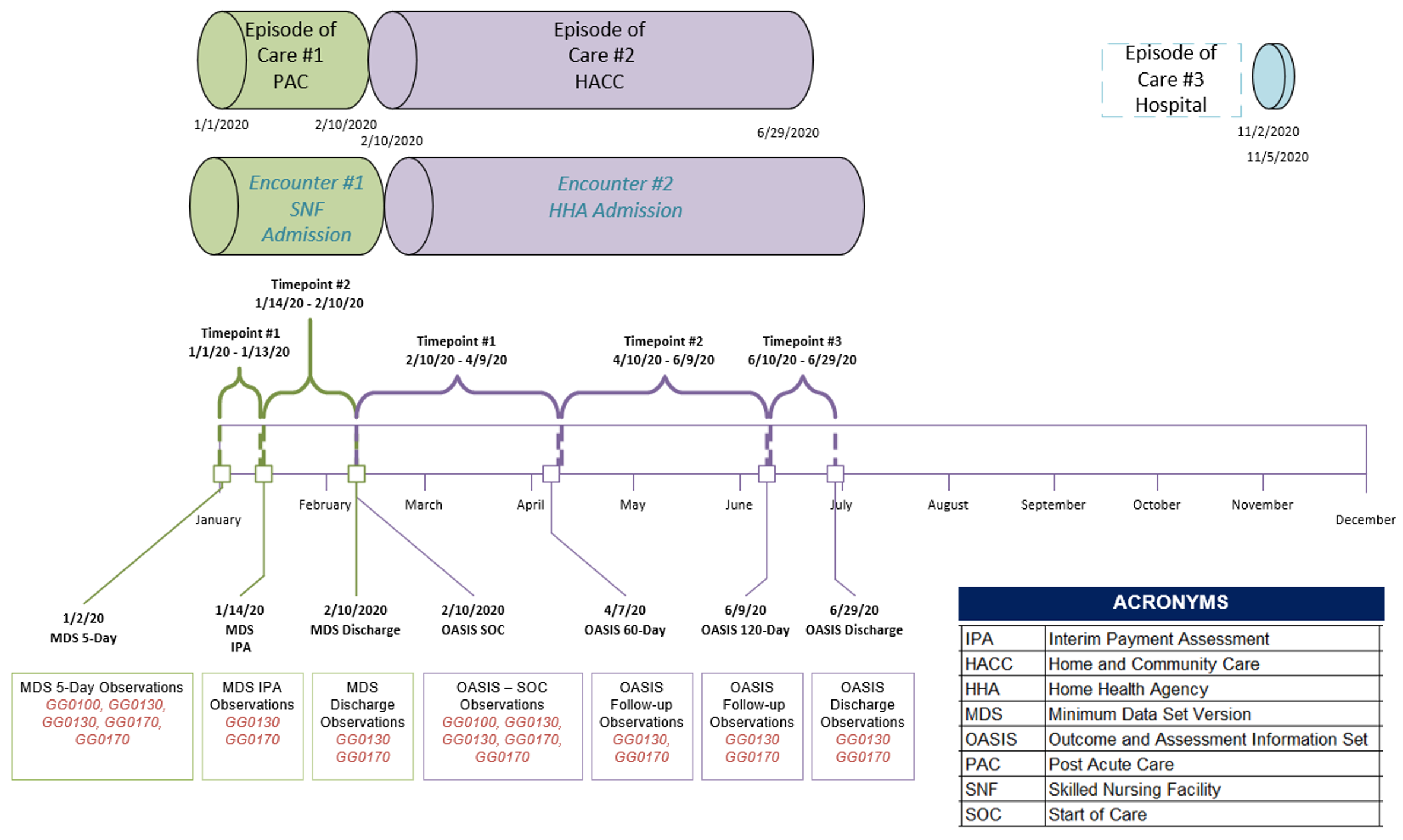
On average, Post-Acute Admissions extend over much longer periods of time than the encounters in the Acute and Ambulatory Care Settings, often going for several months or even years. Over the course of these time periods, the patient condition and therefore the care provided is changing constantly. For example, in Home Health the goal is rehabilitation; Care Plans, Medications, and Orders all likely are changing throughout an admission that could last several months. Already in existence within post-acute care settings are periods of time structured by a variety of stakeholders, some more rigid than others, such as regulations and conditions of participation, payer and revenue cycle requirements, and provider specific processes and protocols.
In settings like home health and skilled nursing facilities (SNFs), there are Medicare assessment instruments that providers must complete at specified intervals that vary by care setting; the results of these assessments drive the Care Plan until a subsequent assessment. If a patient has a pain management Care Plan, and their pain levels improve, then they may have their Opioid drug dosages reduced or eliminated. If the patient's ambulation is improving, then the care team may focus interventions on more complex exercises. These periods of time, defined by many different drivers, have direct impact on how data is made available outside of an EMR. Without a structure in place to hold this information, a connecting application or patient would have to sift through months of information rather than focusing on a given period or periods most relevant to the needs of the application, patient, or other entity.
Out of hospital care spans longer periods of time than in Acute and Ambulatory settings of care. Where a patient may have a 1 hour annual check up with their Primary Care Provider (PCP), a Home Health nurse may see that same patient several times and for several hours at a time each week for months. Within these extended periods of time that make up a Post-Acute admission, there are sub units of time already defined and driven by regulation, payer requirements, and internal processes that organize updates and changes to care being provided. Re-assessment timepoints act as an additional layer of organization within an encounter to help clinicians navigate the volume of data in a long-term encounter to more easily parse the specific information they may be seeking.
For example, at the start of a Home Health admission, the patient may be transitioning from an acute event and have care plans and other clinical considerations to meet their needs at that time; whereas at the end of the admission (several weeks later) the patient may have rehabilitated and the care plan, medications, diagnosis, and other key clinical data points may have changed significantly. Currently, there is no FHIR structure to build out these sub-units of a broader home health admission to properly define the progression of care.
We have selected the Encounter Resource for the Re-assessment Timepoints profile. to this decision included providers, health IT organizations, HL7® workgroups and HL7® FHIR® subject matter experts, governing bodies such as CMS, LOINC Contributors, and others.

The PACIO Project is a collaborative effort to advance interoperable health data exchange between post-acute care (PAC) and other providers, patients, and key stakeholders across health care and to promote health data exchange in collaboration with policy makers, standards organizations, and industry through a consensus-based approach.
The primary goal of the PACIO Project is to establish a framework for the development of Fast Healthcare Interoperability Resource (FHIR®) technical implementation guides and reference implementations that will facilitate health data exchange through standards-based use case-driven application programming interfaces (APIs).
The audience for this IG includes architects and developers of healthcare information technology (HIT) systems in the US Realm that exchange clinical and non-clinical data. Business analysts and policy managers also might benefit from a basic understanding of the use of FHIR® profiles across multiple implementation use cases. Finally, Quality Reporting Agencies, Standards Development Organizations (SDOs), Payors, Providers and Patients will benefit from this IG.
This IG is divided into several pages which are listed at the top of each page in the menu bar.
| Term | Definition |
|---|---|
| Use case | A use case is a list of technical actions or event steps typically defining the interactions between a role and a system to achieve a goal. The actor can be a human or other external system. These technical scenarios describe systems interactions between technical actors to implement the business case. |
| Re-assessment timepoint | A more consumable time block of a broader Post-Acute admission to properly define the progression of care over time for an encounter or episode of care. |