Da Vinci Prior Authorization Support (PAS) FHIR IG, published by HL7 International / Financial Management. This guide is not an authorized publication; it is the continuous build for version 2.2.0 built by the FHIR (HL7® FHIR® Standard) CI Build. This version is based on the current content of https://github.com/HL7/davinci-pas/ and changes regularly. See the Directory of published versions
| Official URL: http://hl7.org/fhir/us/davinci-pas/ImplementationGuide/hl7.fhir.us.davinci-pas | Version: 2.2.0 | ||||
| IG Standards status: Trial-use Active as of 2026-03-02 | Maturity Level: 4 | Computable Name: DaVinciPriorAuthorizationSupport | |||
| Other Identifiers: OID:2.16.840.1.113883.4.642.40.24 | |||||
Welcome to the post-ballot public review for the STU 2.2 release of the Da Vinci Prior Authorization (PAS) implementation guide.
As a result of ballot feedback, a number of additional changes have been made to the IG, some of them substantive. Because of these substantive changes, we're providing an opportunity for the community to perform an additional layer of review to the changes. Feedback on this release should be limited to only those aspects of the specification changed since the ballot, though technical corrections identifying issues with spelling, grammar, formatting, broken links, etc. are welcome for any portion of the specification. Feedback submitted against other parts of the specification will likely be deferred to a future release, particularly if they would involve substantive change, though all feedback provided will be considered at some point.
Feedback on changes made since the ballot will generally fall into one of two categories:
- The change was not made as agreed or accidentally introduced a new issue. (Please check for situations where an agreed change was subsequently overridden by a subsequent change.)
- The commenter disagrees with some of the changes made. While the project can revisit decisions, doing so requires convincing new arguments not already discussed and considered by the regular project calls. Therefore, be sure to provide clear justification for any request to revisit and be aware that those attending the calls may quickly find the issue non-persuasive if there have not been new, not previously discussed, considerations identified.
Feedback should be provided using HL7's Jira mechanism, though discussion on the PAS Zulip stream is also welcome.
This specification is currently published as a Standard for Trial Use (STU).
Note that this implementation guide is intended to support mapping between FHIR and X12 transactions. To respect X12 intellectual property, all mapping and X12-specific terminology information will be solely published by X12 and made available in accordance with X12 rules - which may require membership and/or payment. Please see this Da Vinci External Reference page for details on how to get this mapping.
The specific X12 transactions that this IG supports are 005010X217 - Health Care Services Review - Request for Review and Response (278) and 005010X215 - Health Care Services Review - Inquiry and Response (278). There are many situationally required fields that are specified in those guides that do not have guidance in this Implementation Guide. All of these fields are marked as Must Support in this guide. However, due to licensing restrictions, implementers need to consult the above X12 guides to know the requirements for these fields.
Several of the profiles will require use of terminologies that are part of X12 which we anticipate being made publicly available. At such time as this occurs, the implementation guide will be updated to bind to these as external terminologies.
Prior authorization is a process commonly used by payer organizations to manage healthcare costs. However, the process of requesting and receiving prior authorizations can be slow and inefficient. The Administrative Simplification provisions of HIPAA mandate that the X12 278 Health Care Services Review Request for Review and Response be used for communicating prior authorization requests and responses. While few electronic health record (EHR) systems have implemented this interface, this functionality is often implemented as a portal solution and/or as a part of Practice Management and Revenue Cycle Management solutions. As a result, prior authorizations are often solicited by fax or by using payer-specific portals where clinicians re-key relevant information. Fax submission requires manual transcription on the payer side and may result in significant back-and-forth requesting additional information prior to a decision being made. Re-keying information is inefficient and can result in data entry errors.
This implementation guide strives to enable direct submission of prior authorization requests from EHR systems using a standard already widely supported by most EHRs - FHIR. To meet regulatory requirements, these FHIR interfaces will communicate with an intermediary who, when necessary, can convert the FHIR requests to the corresponding X12 instances prior to passing the requests to the payer. Responses are handled by a reverse mechanism (payer to intermediary as X12, then converted to FHIR and passed to the EHR). Direct submission of prior authorization requests from the EHR will reduce costs for both providers and payers. It will also result in faster prior authorization decisions which will lead to improved patient care and experience.
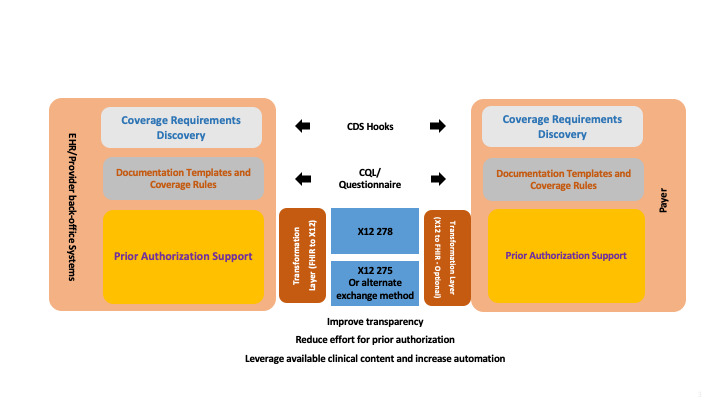
When combined with the Da Vinci Coverage Requirements Discovery (CRD) and Documentation Templates and Rules (DTR) implementation guides, direct submission of prior authorization requests will further increase efficiency by ensuring that authorizations are always sent when (and only when) necessary, and that such requests will almost always contain all relevant information needed to make the authorization decision on initial submission.
The implementation guide also defines capabilities around the management of prior authorization requests, including checking the status of a previously submitted request, updating a previously submitted request, and canceling a request.
A high-level summary of how all of these IGs will work together can be seen below:
When using PAS under the CMS granted exception (Request Number: HL7 FHIR Exception #2021031001), the implementer(s) can disregard any requirements in this Implementation Guide to translate the PAS FHIR Bundle into or out of the X12 278. The defined PAS FHIR request bundles can then be transmitted intact between the provider and payer. The PAS FHIR response bundles can also be transmitted intact between the payer and the provider. NOTE: This CMS exception has ended as of June 2024.
The Office of Burden Reduction and Health Informatics (OBRHI) National Standards Group (NSG) announced an enforcement discretion that they would not enforce the requirement to use the X12 278 for prior authorization if the covered entities were using the Fast Healthcare Interoperability Resources (FHIR) based Prior Authorization API as described in the CMS Interoperability and Prior Authorization final rule (CMS-0057-F). This allows the payer to return a prior authorization number for use in the X12 837 in coverage extension of the CRD and DTR IGs or as part of the all FHIR exchange of the Prior Authorization Response Bundle in the PAS IG.
When covered entities are operating under the enforcement discretion, the trading partners can disregard any requirements in this Implementation Guide to translate the PAS FHIR Bundle into or out of the X12 278. The defined PAS FHIR request bundles can then be transmitted intact between the provider and payer. The PAS FHIR response bundles can also be be transmitted intact between the payer and the provider.
This implementation guide (and the menu for it) is organized into the following sections:
At present, PAS is based on FHIR R4. In addition, PAS is dependent on the US Core 3.1 (FHIR R4), US Core 6.1 (FHIR R4) and US Core 7.0 (FHIR R4) implementation guides. The first is supported for those systems limited to USCDI 1 capabilities, the second is for upcoming regulatory requirements mandating support for USCDI 3, and the last is to enable support for proposed regulations mandating support for USCDI 4. Wherever possible, Da Vinci profiles strive to comply with all three releases, simplifying implementation for those who will need to support varying regulatory expectations over time. In some situations, the payer community requires additional constraints or needs to profile resources that are not yet supported by US Core. In these cases, this IG does not derive from the US Core profiles, though it does align with them as much as possible. It is possible that certain PAS profiles and/or descriptive content may migrate to a future release of US Core, and in some cases, to the base FHIR standard.
In addition, this guide uses content from the following FHIR-related specifications and implementation guides:
In addition, this guide also relies on a number of parent implementation guides:
| Implementation Guide | Version(s) | Reason |
|---|---|---|
| CARIN Consumer Directed Payer Data Exchange (CARIN IG for Blue Button®) | 2.0.0 | Imported by Da Vinci Prior Authorization Support (PAS) FHIR IG (and potentially others) |
| CDS Hooks | 3.0.0-ballot | Imported by Da Vinci - Coverage Requirements Discovery (and potentially others) |
| CDS Hooks Library | 1.0.1 | Imported by Da Vinci - Coverage Requirements Discovery (and potentially others) |
| Da Vinci - Coverage Requirements Discovery | current | |
| 2.1.0 | Imported by Da Vinci - Documentation Templates and Rules (and potentially others) | |
| 2.0.0 | Imported by Da Vinci Prior Authorization Support (PAS) FHIR IG (and potentially others) | |
| Da Vinci - Documentation Templates and Rules | current | |
| 2.1.0 | Imported by Da Vinci Clinical Data Exchange (CDex) (and potentially others) | |
| Da Vinci Clinical Data Exchange (CDex) | 2.1.0 | |
| Da Vinci Health Record Exchange (HRex) | current | Imported by Da Vinci - Coverage Requirements Discovery (and potentially others) |
| 1.1.0 | Imported by Da Vinci - Coverage Requirements Discovery (and potentially others) | |
| 1.0.0 | Imported by Da Vinci - Coverage Requirements Discovery (and potentially others) | |
| Da Vinci Prior Authorization Support (PAS) FHIR IG | 2.1.0 | Imported by Da Vinci - Documentation Templates and Rules (and potentially others) |
| FHIR Extensions Pack | 5.3.0-ballot-tc1 | Imported by Structured Data Capture (and potentially others) |
| 5.2.0 | Automatically added as a dependency - all IGs depend on the HL7 Extension Pack | |
| 5.1.0 | Imported by Da Vinci - Coverage Requirements Discovery (and potentially others) | |
| 1.0.0 | Imported by Da Vinci - Coverage Requirements Discovery (and potentially others) | |
| FHIR R4 package : Core | 4.0.1 | Imported by HL7 Terminology (THO) (and potentially others) |
| FHIR Tooling Extensions IG | current | Imported by Da Vinci Health Record Exchange (HRex) (and potentially others) |
| 1.0.0 | Imported by Da Vinci - Coverage Requirements Discovery (and potentially others) | |
| HL7 Terminology (THO) | 7.0.1 | Automatically added as a dependency - all IGs depend on HL7 Terminology |
| 6.5.0 | Imported by FHIR Extensions Pack (and potentially others) | |
| 6.2.0 | Imported by CDS Hooks Library (and potentially others) | |
| 6.1.0 | Imported by Da Vinci - Coverage Requirements Discovery (and potentially others) | |
| 5.5.0 | Imported by US Core (and potentially others) | |
| 5.3.0 | Imported by Da Vinci - Coverage Requirements Discovery (and potentially others) | |
| 5.0.0 | Imported by Subscriptions R5 Backport (and potentially others) | |
| Public Health Information Network Vocabulary Access and Distribution System (PHIN VADS) | 0.12.0 | Imported by US Core (and potentially others) |
| SMART App Launch | 2.0.0 | Imported by US Core (and potentially others) |
| Security for Scalable Registration, Authentication, and Authorization | 0.1.0 | Imported by Da Vinci Health Record Exchange (HRex) (and potentially others) |
| Structured Data Capture | current | Imported by Da Vinci - Documentation Templates and Rules (and potentially others) |
| 3.0.0 | Needed for referencing the US-Core QuestionnaireResponse profile | |
| Subscriptions R5 Backport | 1.1.0 | Imported by Da Vinci Prior Authorization Support (PAS) FHIR IG (and potentially others) |
| US Core | 7.0.0 | Needed for systems supporting USCDI v4 |
| 6.1.0 | Needed for systems supporting USCDI v3 | |
| 3.1.1 | Needed for systems supporting USCDI v1 | |
| Value Set Authority Center (VSAC) | 0.7.0 | Imported by CARIN Consumer Directed Payer Data Exchange (CARIN IG for Blue Button®) (and potentially others) |
| 0.19.0 | Imported by Da Vinci Health Record Exchange (HRex) (and potentially others) | |
| 0.18.0 | Imported by US Core (and potentially others) | |
| 0.11.0 | Imported by Da Vinci - Coverage Requirements Discovery (and potentially others) |
| Parameter | Value |
|---|---|
| system-version | SNOMED CT[US] |
This implementation guide defines additional constraints and usage expectations above and beyond the information found in these base specifications.
This implementation guide and the underlying FHIR specification are licensed as public domain under the FHIR license. The license page also describes rules for the use of the FHIR name and logo.
There are a number of X12 codes that are used in the examples in this Implementation Guide. These codes are listed within an X12 implementation guide and maintained by X12. All X12 work products are copyrighted. See their website for licensing terms and conditions.
CPT © Copyright 2026 American Medical Association. All rights reserved. AMA and CPT are registered trademarks of the American Medical Association.
This publication includes IP covered under the following statements.