HL7 Europe Imaging Study Report, published by HL7 Europe. This guide is not an authorized publication; it is the continuous build for version 0.1.0-build built by the FHIR (HL7® FHIR® Standard) CI Build. This version is based on the current content of https://github.com/bvdh/bvdh-hl7eu-imaging/ and changes regularly. See the Directory of published versions
The imaging report represents a report made by a radiologist based on an imaging study.
The figure below illustrates the structure of the Imaging Report.
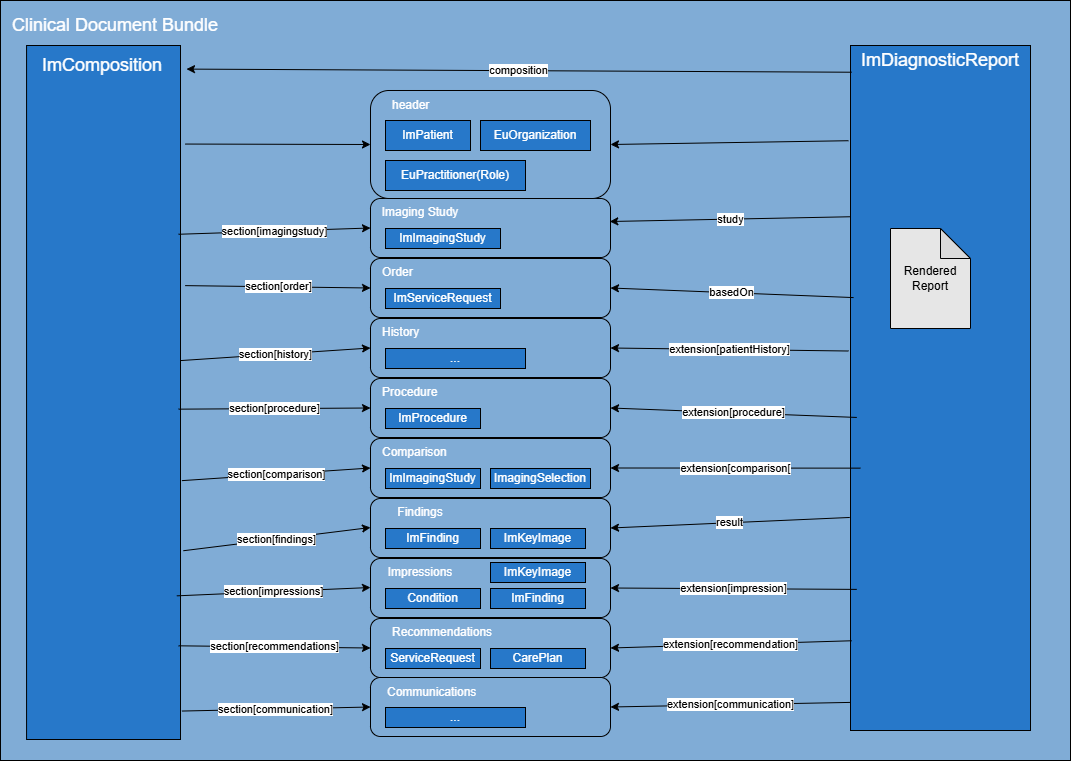
An Imaging Report is a FHIR Clinical Document that contains both a DiagnosticReport as a Composition resource.
The report uses the ImDiagnosticReport to store the structured data. This resource might also include a rendered version of the document. The ImComposition resource is used to present a rendered version of the document as a FHIR document.
As described by IHE-IDR, the all radiology reports contain similar information. This specification reuses this subdivision to label the structured data (see ImDiagnosticReport and recommends it as the structure for sections defined in the ImComposition).
General information on the report. Most of the information elements in this part of the report overlap with other clinical reports. The document header includes information on the patient, source organization, author, attester and custodian of the report.
Information on the studies that this report is reporting on. It includes such as the study identifiers, date and time the exam was done, the modalities used in the exam and the different series. In this implementation guide this is represented by the ImImagingStudy profile.
The order section contains information on the orders that resulted in the studies and this report. It includes information such as the AccessionNumber, the identity of the referring physician or organization, the indication for examination, and, ideally, additional patient context and specific clinical questions provided by the referring physician. Clinical questions are sometimes of the form “Follow-up X”, where X is an existing known finding (perhaps from a previous exam), or “Rule out X”, where X is a condition for which imaging input is requested on whether or not it is present. Indications are also, hopefully, provided to provide important clinical context to the imaging clinician, and to support assessment of the appropriateness of the order and/or billing. If indications are not present, they are sometimes sought out by imaging staff.
Note: “Rule out X”, while somewhat helpful for the imaging clinician, can be problematic for billing since the symptoms that suggest the possible presence of the condition and establish the medical necessity of the imaging exam are implied, but not captured. Site practices increasingly deprecate such wording.
In this specification, the order is represented by the ImOrder profile.
This section includes patient history and other prior clinical details deemed relevant to the imaging study by the imaging clinician. Some information may be provided by the referring physician in the order, and more is extracted from the medical record by imaging staff, automated tools, or by the radiologist themselves. This information provides background for the imaging clinician, context for the contents of the report, and is sometimes relevant to billing and clinical guidelines. Potential sources include impressions or summaries of the clinical notes from the encounter where the imaging order was placed.
This section contains information such as the procedure type, the anatomy imaged, the date and time of the imaging examination, and the facility that performed it.
Also called Imaging technique, this section may describe the parameters that were used, details of any contrast media and/or radiopharmaceuticals administered, including concentration, volume, and route of administration, and any medications, and catheters or devices used.
The section can also describe preparation of the data produced by the procedure: Views, image sets, recons, reformats and post processing.
Radiation dose may also be described here; the text content and metrics may be constrained/formatted to meet local regulations.
The information in this section is typically more detailed than what is listed as the Order, and in fact may differ from the ordered exam based on the needs of the patient and the judgment of the imaging clinician.
Any deficiencies of the study may also be described here, such as whether the imaging was incomplete or if there were quality issues that prevented interpretation of some part of the study or otherwise compromise the sensitivity and specificity of the examination. In the event that a patient was unable to undergo imaging, for example due to claustrophobia or a seizure, a report might still be produced and this section would note that the exam was not performed and provide a reason.
While the actual instructions given to the patient are not typically listed in the report, some mention the fact that instructions were given, and perhaps that risks were discussed, and consent was obtained. Procedure notes from the technologist are typically captured elsewhere, but significant details such as adverse patient reactions, or things that may affect the quality of the study, may be included here.
Procedure details that may be required for billing are sometimes included here as well.
In this specification, this information is represented by the ImProcedure profile.
This section is a list of other studies that were considered relevant by the imaging clinician. They are typically identified by type (modality, anatomy, exam type) and date. Findings from these studies and comparisons with the current study are typically woven into the next section (e.g. indicating no change, differentiating descriptions and/or measurements), although some of these studies may not be specifically mentioned in the findings. It is typically presumed that both the images and the report for each comparison study were available to the imaging clinician, however in some cases, such as for external priors, only the report or only the images were available, in which case that may be noted here.
In this specification a comparison study can be represented as an ImImagingStudy describing the full study or an ImagingSelection resource representing part of a study.
This section provides a detailed description of the findings on the imaging examination. The findings should be described in a clear and concise manner, using standardized anatomic, pathologic, and radiologic terminology whenever possible.
When there are significant numbers of findings, the imaging clinician will typically organize them into groups, typically by anatomy. Reporting templates for particular procedure types (such as those at radreport.org) will also often organize the findings.
An important distinction between Findings and Impressions is that Findings capture what the imaging clinician saw in the image, while Impressions capture what they inferred/concluded. The findings might record a radiolucency, while the impression records a fracture. There are some cases where the two overlap, but generally imaging clinicians try to capture in the Findings what the significant image features are and strive in the Impressions to communicate to the referring physician what they think those represent in clinical terms.
In this specification, findings are represented as resources following the ImFinding profile. Optionally, this section can also hold one or more key image resource represented by either ImKeyImageImagingSelection or ImKeyImageDocumentReference.
Sometimes also called Conclusion or Diagnosis, provides the radiologist’s overall interpretation of the findings, a specific diagnosis and/or differential diagnosis (when possible), responses to any clinical questions posed by the referring physician, and any recommendations for further management and/or confirmation, as appropriate.
Recommendations most often cover subsequent diagnostic imaging or other diagnostic procedures such as biopsies or lab tests. They may also include suggestions to correlate the imaging result with other clinical information to improve the confidence of the diagnosis, referrals to specialists, or less commonly, therapeutic procedures. The recommendations may cite specific guidelines applied, particularly when the referring physician might be less familiar with the current guidelines for certain findings than the imaging clinician. The imaging clinician may take into account the expertise of the referring physician when composing recommendations; for an unusual cancer, a family physician might find follow-up recommendations more helpful than an oncology specialist would.
Since referring physicians may specifically focus their attention on this section, the imaging clinician may choose particularly important details such as key findings or any adverse events, to re-iterate and summarize here.
The order of items in the impression is often significant, in that imaging clinicians frequently put the most critical, most actionable, most significant items first in the impression section to minimize the chance of them being overlooked. In the case of differential diagnosis, the multiple possible diagnoses are typically presented in order from the most likely to the least likely. Impression items may also be numbered to facilitate verbal referencing or linking to communications.
Some items in the impression may be clinically significant but were not associated with the indications or reason for exam; for example, a lung nodule deemed to be suspicious on a chest exam for trauma. These are often referred to as “incidental findings”.
Some items in the impression may be critical, in that they represent the potential for severe negative clinical impact to the patient if appropriate action is not taken promptly. The presence of such items almost always results in a communication with care staff and/or the patient.
In this specification, impressions are represented by ImFinding and Condition resources.
Some items in the impression may be considered actionable, in that some follow-up action or communication is advisable. The recommendations may or may not include a specific corresponding follow-up action. A corresponding communication to relevant persons may or may not have taken place during the reporting process and be noted in the report. In this specification, recommendations are represented as orders (ServiceRequest resources) or CarePlans.
This is an optional section as it not anticipated that it is often required.
There is strong interest in tooling to facilitate communicating critical results clearly and rapidly with the appropriate people, confirming that follow-up of actionable findings takes place, and making sure that incidental findings do not “fall through the cracks”.
Communications are records in the report about attempted and/or successful communications of some content of the report to the referring physician, the patient, or other appropriate person. These communications are initiated during the generation of the DiagnosticReport by members of the organization fulfilling that order. E.g. direct communication of time critical results by the radiologist to the referring physician.
Communication is not listed as a separate section in the ACR guidance, but codes for a communication section do exist. It is common practice to present communication records at the bottom of the report, just below the impressions, since they are often driven by specific items in the impression and occur at the end of the report creation process. Such communication records support medico-legal usage and the review and improvement of conformance to best practices for patient safety and quality of care.
The communication entry typically records the date, time, and method of communication, the person/organization contacted, and may summarize the content communicated.
Typically a Communication resources is used to represent such event.
These define the FHIR resources for systems conforming to this implementation guide:
| Name | Title | Description |
| ImComposition | Composition: Imaging Report | Clinical document used to represent a Imaging Study Report for the scope of the HL7 Europe project. |
| ImDiagnosticReport | DiagnosticReport: Imaging Report | DiagnosticReport profile for Imaging Reports. This document represents the report of an imaging study. It is the anchor resource that refers to all structured data as well as the |
| ImReport | Bundle: Imaging Report | Document Bundle for Imaging Report |
| ImAccessionNumberIdentifier | Identifier: Accession Number | This profile on Identifier represents the Accession Number for the Imaging Order. Within a Hospital Information System environment, accession numbers will usually uniquely identify a manifest or report but are not required to always map 1:1 with a report or manifest due to certain imaging workflows. The imaging report may not be uniquely identified by accession number in an overread scenario (two radiologists reading a single imaging study). The manifest may not be uniquely identified by accession number in the case that the RIS imaging request (accession number assigner) requires two imaging modalities to perform the exam, and thus produces two image manifests. In order to ensure uniqueness across Hospital Information Systems, accession numbers are required to have a system value that identifies the namespace for the issuing authority (ensuring their global uniqueness). |
| ImAdverseEvent | AdverseEvent: Imaging Adverse Event | Adverse Event that occurred during an imaging procedure. |
| ImDiagnosticReportReference | Document DiagnosticReport Reference | This extension provides a reference to the DiagnosticReport instance that is associated with this Composition. |
| ImFinding | Observation: Imaging Finding | Finding during imaging procedure. |
| ImGestationalAgeObservation | Observation: Gestational Age | Gestational Age Observation |
| ImImagingDevice | Device: Imaging Device | The device the made the image. |
| ImImagingSelection | ImagingSelection: General | Imaging Selection |
| ImImagingStudy | ImagingStudy: General | This profile represents an imaging study instance. |
| ImImagingStudyInstanceDescription | Instance Description | A description of the instance in an ImagingStudy. |
| ImKeyImageDocumentReference | DocumentReference: Key Image | A document containing key images for a patient. It can refer to a DICOM or non-DICOM image. When referring to a DICOM image, the DocumentReference.content.attachment.url should be a WADO-URI. When referring to a non-DICOM image, the DocumentReference.content.attachment.url should be a direct URL to the image. When the resource represents a DICOM instance it SHALL contain a the SOP Instance UID in the identifier element. When the resource represents a DICOM series it SHALL contain the Series Instance UID in the identifier element. |
| ImKeyImageImagingSelection | ImagingSelection: Key Image | Key images represented as an ImagingSelection |
| ImOrder | ServiceRequest: Imaging Order | This profile on ServiceRequest represents the order for the Imaging Study and report. |
| ImProcedure | Procedure: Imaging Acquisition | This profile on Procedure represents the imaging procedure. |
| ImRadiationDoseObservation | Observation: Radiation Dose | A record for the radiation dose the subject has been exposed to during an imaging procedure. E.g. based on information from https://dicom.nema.org/medical/dicom/current/output/html/part16.html and https://build.fhir.org/ig/HL7/fhir-radiation-dose-summary-ig/index.html |
| ImReportDocumentReference | DocumentReference: -MHD Imaging Report | A DocumentReference profile for the Report DocumentReference used in MHD deployments. |
| ImSopInstanceUidIdentifier | Identifier: SOP Instance UID | This profile on Identifier represents the SOP Instance UID (0008,0018) for the Imaging Order. |
| ImSrInstanceImagingSelection | ImagingSelection: DICOM SR Instance | Imaging Selection referring to a DICOM SR instance |
| ImStudyInstanceUidIdentifier | Identifier: Study Instance UID | This profile on Identifier represents the Study Instance UID (0020,000D) for the Imaging Order. |