Da Vinci Value-Based Performance Reporting Implementation Guide, published by HL7 International / Clinical Quality Information. This guide is not an authorized publication; it is the continuous build for version 1.1.0 built by the FHIR (HL7® FHIR® Standard) CI Build. This version is based on the current content of https://github.com/HL7/davinci-vbpr/ and changes regularly. See the Directory of published versions
| Page standards status: Informative |
Originally, value-based payment models were designed to reward healthcare providers with incentive payments for the quality of care they give to people with Medicare. The programs were designed to link provider performance of quality measures to provider payment and work with other CMS quality efforts to ensure that quality is being achieved. Value-based purchasing refers to a broad set of performance-based payment strategies that link financial incentives to providers’ performance on a set of defined metrics and measures. Value-based purchasing programs are private or public programs that link financial reimbursement to performance on measures of quality (i.e., structure, process, outcomes, access, and patient experience) and cost or resource use.1
Economic challenges and higher healthcare costs have expanded these value-based payment models to larger populations of patients and members. The industry has adopted several names for the original value-based payment models, including value-based purchasing, value-based contracting, value-based payments, and, most recently, alternative payment models.
For the purpose of this implementation guide, any report that meets the definition of a value-based payment model, meaning a contract that links financial incentives to providers’ financial, quality, and risk performance on defined metrics and measures, will be considered a value-based performance report. Reporting performance against the specific details of a contract may include financial, quality, utilization, etc. over defined time periods.
In this implementation guide, we use the term metrics to refer to financial measures in the report, and the term quality measures or measures to refer to the quality measures such as the colorectal cancer screening measure.
This following is a list of pre-requisites for using this implementation guide:
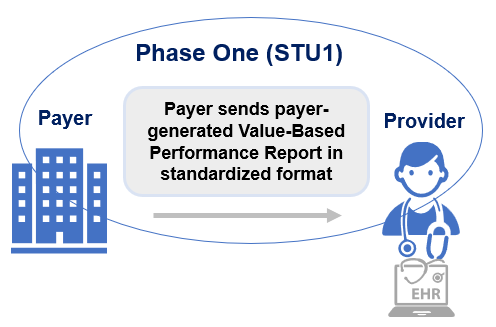
The actors involved in exchanging value-based performance reports are Clients and Servers.
The goals of implementation guide are:
The initial phase of this implementation guide focuses on: