Da Vinci PDex Plan Net, published by HL7 International / Financial Management. This guide is not an authorized publication; it is the continuous build for version 1.2.0 built by the FHIR (HL7® FHIR® Standard) CI Build. This version is based on the current content of https://github.com/HL7/davinci-pdex-plan-net/ and changes regularly. See the Directory of published versions
| Official URL: http://hl7.org/fhir/us/davinci-pdex-plan-net/ImplementationGuide/hl7.fhir.us.davinci-pdex-plan-net | Version: 1.2.0 | |||
| IG Standards status: Trial-use | Computable Name: DaVinciPDEXPlanNet | |||
This implementation guide defines a FHIR interface to a health insurer's insurance plans, their associated networks, and the organizations and providers that participate in these networks. Publication of this data through a standard FHIR-based API will enable third parties to develop applications through which consumers and providers can query the participants in a payer's network that may provide services that address their health care needs. Although there are multiple types and sources of providers' directories, including provider organizations (i.e., a hospital listing all its physicians), government (i.e., listing of providers in Medicare), payers (i.e., a health plan's provider network), and third-party entities (such as vendors that maintain provider directories), the focus of this implementation guide is on Payer Provider Directories.
The PDEX Payer Network (or Plan-Net) Implementation Guide is based conceptually on the Validated Healthcare Directory Implementation Guide (VHDir IG), an international standard. The VHDir IG is based on FHIR Version 4.0. It was developed in cooperation with the Office of the National Coordinator for Health Information Technology (ONC) and Federal Health Architecture (FHA) with guidance from HL7 International, the Patient Administration Workgroup, and the HL7 US Realm Steering Committee.
The use of VhDir as the conceptual base for the profiles and extensions in the PDEX Payer Network Implementation Guide is intended to protect implementers of the Plan-Net IG from rework/remapping when the VHDir concept reaches implementation, and becomes a source of data for the PDEX Payer Network. The primary changes from the VHDir IG are to:
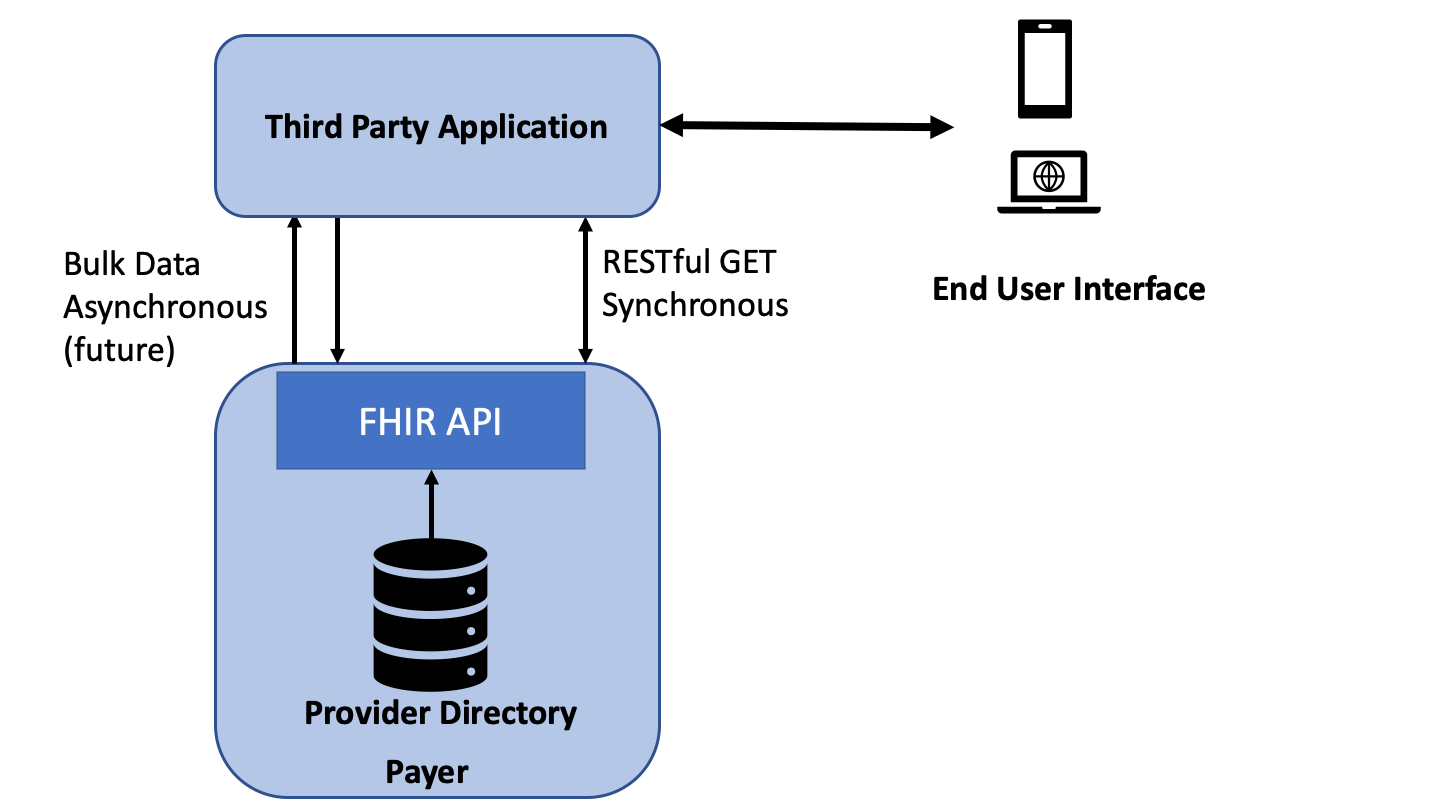
The diagram below depicts the scope of this implementation guide (IG). The IG defines the API that exposes a payer’s provider network (including pharmacy locations where appropriate) for access by a consumer or provider application. This is a query only API (GET) and does not support PUT or POST.
The IG is organized into the following sections:
This implementation guide was written for a US audience and profiles resources from US Core STU 4, where available (Practitioner, Organization and Location), and otherwise from R4 (OrganizationAffiliation, PractitionerRole, HealthCareService, Endpoint). The PractitionerRole profile from US Core was not used because it is over-constrained for use in a Provider Directory based on Payer information. The Network profile is based on USCore Organization, since there was no contradiction between the USCore profile and the Plan-Net requirements. However, the NPI and CLIA identifier types, which are Must-Support, are clearly intended for provider organizations only and are not expected to be populated for other organization types. Alignment with VhDir is maintained by adapting VhDir content, where possible.
Provider directories play a critical role in enabling identification of individual providers and provider organizations, as well as characteristics about them. Provider directories support a variety of use cases, including:
This IG addresses two actors:
For anticipated query use cases, please see Representing and Searching Provider Data.
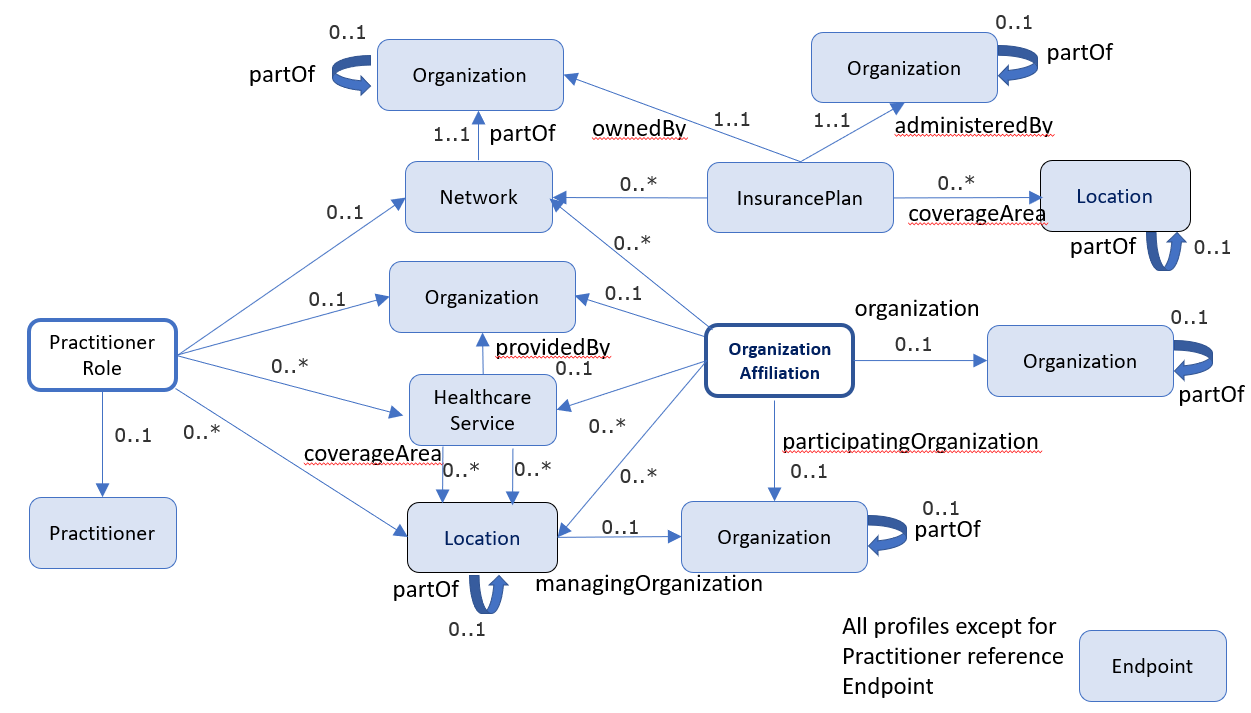
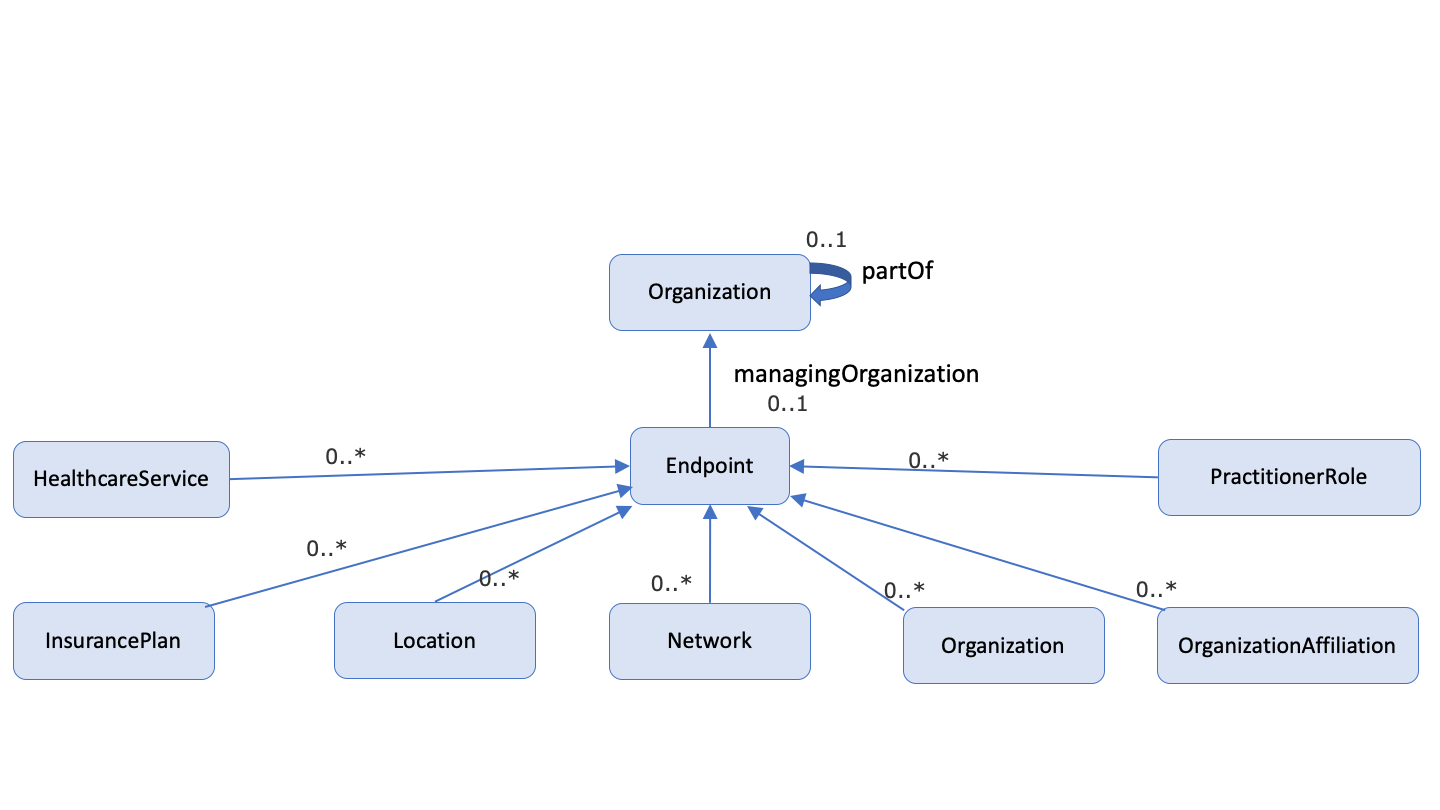
Note: the following diagrams provide a high-level view of the relationships between resources used in this IG. They do not necessarily reflect all of the relationships/references between resources.
This IG was developed by the MITRE Corporation under the direction of the authors using FHIR Shorthand syntax and the SUSHI tookit, a free, open source toolchain from the MITRE Corporation. Generous guidance on FHIR Shorthand and SUSHI was provided by Chris Moesel. The capability statements were developed with support of tools and generous guidance from Eric Haas, and benefited from critical review by Yengibar Manasyan.
Package hl7.fhir.uv.extensions.r4#5.2.0 This IG defines the global extensions - the ones defined for everyone. These extensions are always in scope wherever FHIR is being used (built Mon, Feb 10, 2025 21:45+1100+11:00) |
Package hl7.fhir.uv.extensions.r4#1.0.0 This IG defines the global extensions - the ones defined for everyone. These extensions are always in scope wherever FHIR is being used (built Sun, Mar 26, 2023 08:46+1100+11:00) |
Package hl7.fhir.uv.bulkdata#2.0.0 FHIR based approach for exporting large data sets from a FHIR server to a client application (built Fri, Nov 26, 2021 05:56+1100+11:00) |
Package hl7.fhir.uv.sdc#3.0.0 The SDC specification provides an infrastructure to standardize the capture and expanded use of patient-level data collected within an EHR. |
Package ihe.formatcode.fhir#1.1.0 Implementation Guide for IHE defined FormatCode vocabulary. (built Thu, Feb 24, 2022 16:55-0600-06:00) |
Package hl7.fhir.us.core#6.1.0 The US Core Implementation Guide is based on FHIR Version R4 and defines the minimum conformance requirements for accessing patient data. The Argonaut pilot implementations, ONC 2015 Edition Common Clinical Data Set (CCDS), and ONC U.S. Core Data for Interoperability (USCDI) v1 provided the requirements for this guide. The prior Argonaut search and vocabulary requirements, based on FHIR DSTU2, are updated in this guide to support FHIR Version R4. This guide was used as the basis for further testing and guidance by the Argonaut Project Team to provide additional content and guidance specific to Data Query Access for purpose of ONC Certification testing. These profiles are the foundation for future US Realm FHIR implementation guides. In addition to Argonaut, they are used by DAF-Research, QI-Core, and CIMI. Under the guidance of HL7 and the HL7 US Realm Steering Committee, the content will expand in future versions to meet the needs specific to the US Realm. These requirements were originally developed, balloted, and published in FHIR DSTU2 as part of the Office of the National Coordinator for Health Information Technology (ONC) sponsored Data Access Framework (DAF) project. For more information on how DAF became US Core see the US Core change notes. (built Fri, Jun 30, 2023 14:02+0000+00:00) |
Package hl7.fhir.us.core#7.0.0 The US Core Implementation Guide is based on FHIR Version R4 and defines the minimum conformance requirements for accessing patient data. The Argonaut pilot implementations, ONC 2015 Edition Common Clinical Data Set (CCDS), and ONC U.S. Core Data for Interoperability (USCDI) v1 provided the requirements for this guide. The prior Argonaut search and vocabulary requirements, based on FHIR DSTU2, are updated in this guide to support FHIR Version R4. This guide was used as the basis for further testing and guidance by the Argonaut Project Team to provide additional content and guidance specific to Data Query Access for purpose of ONC Certification testing. These profiles are the foundation for future US Realm FHIR implementation guides. In addition to Argonaut, they are used by DAF-Research, QI-Core, and CIMI. Under the guidance of HL7 and the HL7 US Realm Steering Committee, the content will expand in future versions to meet the needs specific to the US Realm. These requirements were originally developed, balloted, and published in FHIR DSTU2 as part of the Office of the National Coordinator for Health Information Technology (ONC) sponsored Data Access Framework (DAF) project. For more information on how DAF became US Core see the US Core change notes. (built Wed, May 8, 2024 15:33+0000+00:00) |
Package hl7.fhir.uv.extensions.r4#5.1.0 This IG defines the global extensions - the ones defined for everyone. These extensions are always in scope wherever FHIR is being used (built Sat, Apr 27, 2024 18:39+1000+10:00) |
Package hl7.fhir.us.davinci-hrex#1.1.0 The Da Vinci Payer Health Record exchange (HRex) Framework/library specifies the FHIR elements used in multiple Da Vinci implementation guides. This includes FHIR profiles, functions, operations, and constraints on other specifications such as CDS-Hooks and other aspects of Da Vinci Use Cases that are common across more than a single use case.\n\nDa Vinci HRex Implementation Guide (IG) will make use of US Core profiles that are based on the FHIR R4 specification wherever practical. The HRex IG will use the HL7 FHIR Release 4/US Core STU3 specification as its base but will provide additional guidance and documentation to support implementations that follow the HL7 FHIR STU3/US Core STU2 and HL7 FHIR DSTU2/Argonaut specifications.\n\nThe HRex profiles documented in this IG will be used to exchange data between providers systems (e.g. EHRs) and other providers, payers, and third-party applications where appropriate. In addition, exchanges from payer systems to providers, other payers, and third-party applications are supported by the HRex profiles and operations.\n\nHRex may define new extensions, profiles, value sets, constraints/extension to other specification (e.g. specific CDS-Hooks) that are specific Da Vinci requirements. Where appropriate these Da Vinci specific artifacts will be promoted for incorporation into the future versions of existing standards (e.g. R4 US Core profiles) and deprecated in this guide on publication in the updated standard. (built Tue, Dec 10, 2024 16:43+0000+00:00) |
This implementation guide and the underlying FHIR specification are licensed as public domain under the FHIR license. The license page also describes rules for the use of the FHIR name and logo.
This publication includes IP covered under the following statements.