Consumer Real-Time Pharmacy Benefit Check FHIR IG, published by HL7 International / Pharmacy. This guide is not an authorized publication; it is the continuous build for version 2.0.0 built by the FHIR (HL7® FHIR® Standard) CI Build. This version is based on the current content of https://github.com/HL7/carin-rtpbc/ and changes regularly. See the Directory of published versions
The real-time pharmacy benefit check (RTPBC) process involves a request from a consumer application used by a patient to either (a) the party that manages the pharmacy benefit portion of the patient's health insurance or (b) a party that serves as a source for typical and discount medication pricing information.
The patient application submits a request containing…
Example: Bundled RTPBC request
The responder…
Example: Bundled RTPBC response from payer/PBM
The patient application submits a request containing…
The responder…
The consumer RTPBC request and response are accomplished using FHIR Claim and ClaimResponse resources in a "predetermination" (what-if) mode. Other FHIR® resources support the exchange by fleshing out patient, prescription, pharmacy and coverage information needed to determine accurate cost and coverage. An OperationOutcome communicates exception situations where a ClaimResponse cannot be returned.
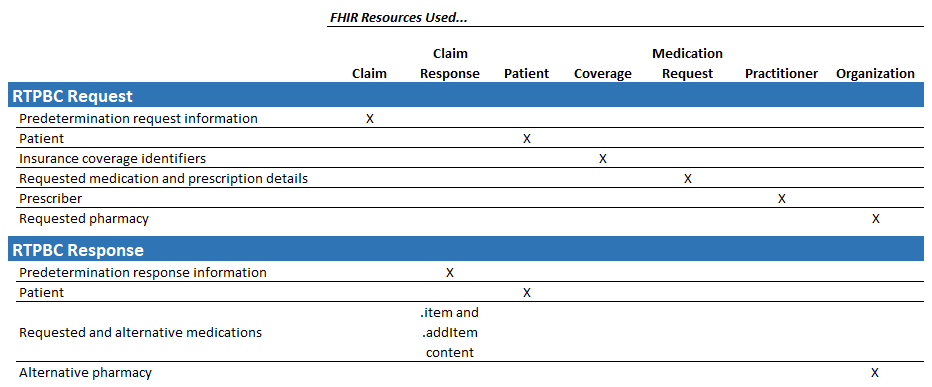
Claim - Represents the RTPBC request. Uses the predetermination Claim.use mode
ClaimResponse - Represents the RTPBC response
Patient - Conveys the patient information needed for the exchange
Coverage - Conveys the patient's pharmacy benefit coverage IDs
MedicationRequest - Conveys the needed prescription information (a subset of what is present in a full prescription)
Organization (Pharmacy) - Conveys pharmacy information needed for the exchange (based on the US Core Organization profile)
Practitioner - Prescriber information is conveyed using the US Core Practitioner profile.