US Medication Risk Evaluation and Mitigation Strategies (REMS) FHIR IG, published by HL7 International / Pharmacy. This guide is not an authorized publication; it is the continuous build for version 2.0.0 built by the FHIR (HL7® FHIR® Standard) CI Build. This version is based on the current content of https://github.com/HL7/fhir-medication-rems-ig/ and changes regularly. See the Directory of published versions
Before reading this formal specification, implementers are encouraged to first familiarize themselves with other key portions of this implementation guide:
The Participant Roles and Needs section overviews the real world people and organizations who participate in REMS programs and defines the system roles referenced in the specification below.
The REMS Steps and Terminology and Use Cases sections describe the process context and goals behind the interactions defined below
The Technical Background page identifies related specifications that this guide depends on.
This implementation guide uses the following terms to set expectations for implementers to conform to specific behaviors and information content it defines:
SHALL indicates requirements that must be met to be conformant with the specification.
SHOULD indicates behaviors that are strongly recommended (and which could result in interoperability issues or sub-optimal behavior if not adhered to), but which are not strictly required for an implementation to be considered conformant to this version of the guide.
MAY describes optional behaviors that implementers are free to consider but where there is no recommendation for or against adoption.
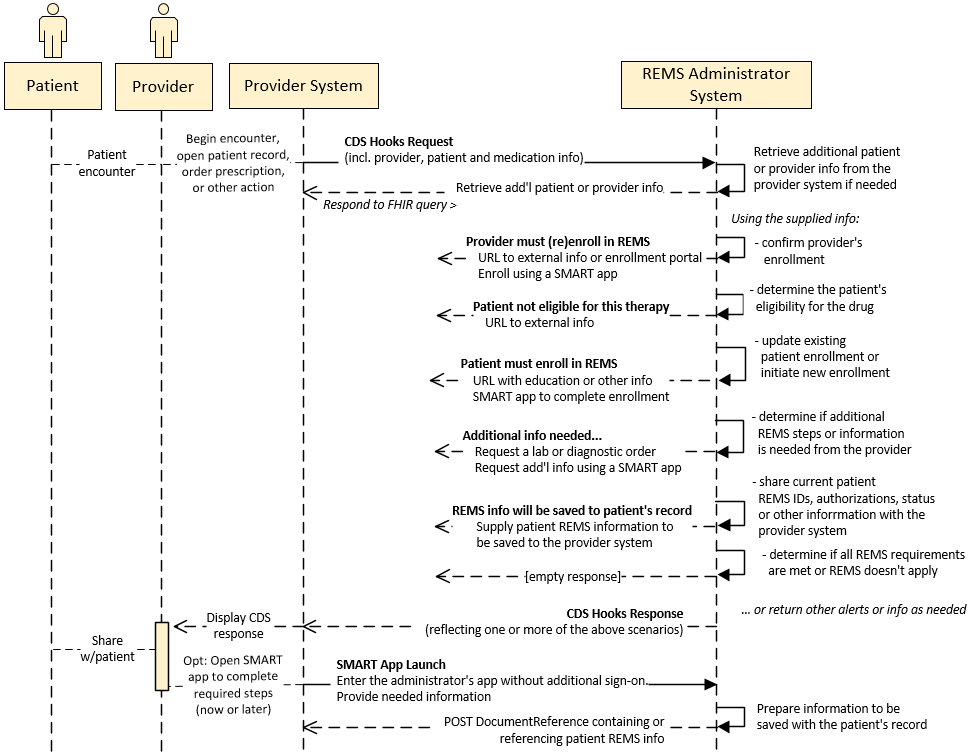
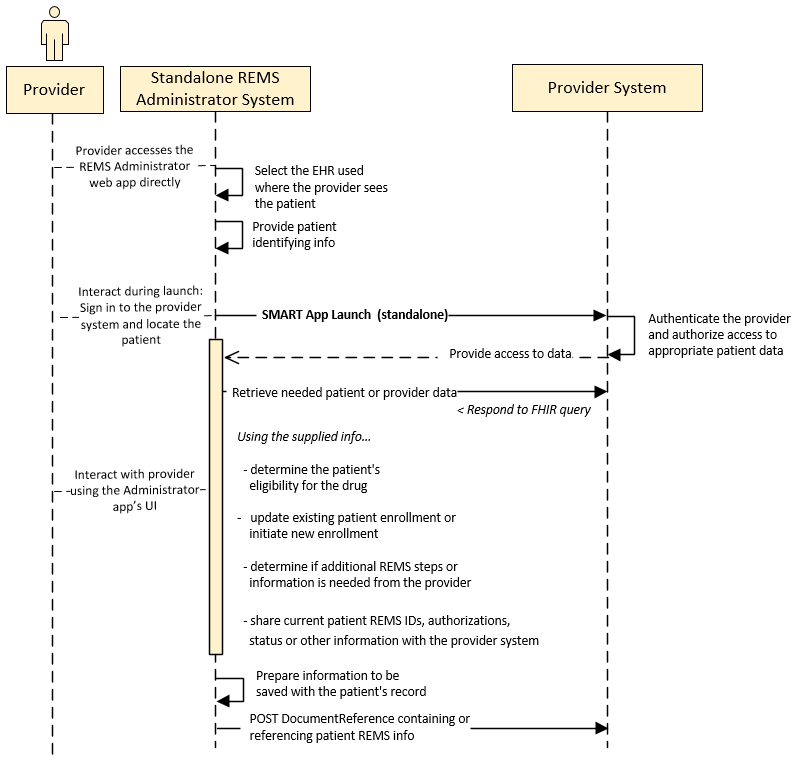
This implementation guide establishes two basic interaction patterns between a Provider System and REMS Administrator System that can be applied at multiple points in treating a patient with a REMS drug:
This interaction is initiated by the Provider System during the provider’s workflow, using CDS Hooks and, optionally, EHR-based SMART App Launch.
In this interaction, a provider uses an external REMS Administrator application that accesses patient data in a Provider System using standalone SMART app launch.
The guide does not strictly require that either of these patterns be implemented at particular workflow events. Implementers are free to choose when and how they apply these interactions. However, implementers SHOULD support these interactions whenever possible to:
In particular, this guide strongly recommends leveraging the CDS Hooks and SMART app launch workflow at the start of the patient’s therapy to raise patient enrollment requirements and enable them to be completed quickly, minimizing manual data entry and preventing a possible delay in treatment.
Many EHRs support a subset of CDS Hooks and SMART launch features today to bring alerts and information into the prescriber’s workflow at appropriate times–to be acted upon immediately.
The guide makes use of these features to notify the prescriber of pertinent REMS information, for example that there’s a REMS program for a drug being considered or that the prescriber’s REMS enrollment has lapsed. The provider’s response in these situations may be to simply acknowledge the information before continuing with their workflow.
A provider may also take the opportunity to complete a REMS requirement returned in a CDS Hooks response immediately through use of a SMART app. Use of the guide’s patterns can minimize the time needed from the provider in such a circumstance–to complete a patient enrollment form, for example–by the REMS Administrator prefilling or hiding questions that were satisfied by data provided in the preceding CDS Hooks interaction.
Provider Systems SHALL support immediate provider responses to Cards returned .
In other cases, a provider action may not be able to be completed immediately upon receiving it in a CDS Hooks response, and instead may need to be deferred until a later time. The guide leverages an approach where the REMS Administrator’s CDS Hooks response includes a suggestion Card containing a Task resource enabling the provider to launch the indicated SMART app later, as described in the CDS Hooks Card Profiles section.
Provider Systems SHOULD support suggestion cards with associated actions to defer the launch of SMART application, and SHOULD provide the REMS Administrator’s CDS server sufficient OAuth scopes to enable the app to create a Task to enable the deferred launch, as described here.
In some situations, it may be helpful for the prescriber or other provider assisting in the care of a REMS patient to manually launch the associated REMS Administrator SMART app, independent of a CDS Hooks interaction.
Provider Systems and REMS Administrators MAY support manual launch of the REMS Administrator SMART application.
When a Provider System provides this support, it SHALL provide patient context during launch.
The REMS Administrator SMART app MAY save information about the patient’s REMS participation to the Provider System’s patient record. Saving of REMS information is typically most effective during the provider’s interaction with a SMART app because it can be timed to occur after activities that might change the patient’s status or information–for example by completing patient enrollment.
To enable this to occur, the Provider System SHOULD authorize a REMS Administrator’s SMART app with sufficient OAuth scopes to enable the app to create a DocumentReference resource associated to the patient. This guidance in the SMART App Launch IG provides details for assigning scopes during app launch.
If using this capability, the REMS Administrators SHOULD follow US Core DocumentReference guidance when creating this resource.
In addition to the US Core requirements, this guide recommends populating DocumentReference.type with the LOINC value 51851-4 (Administrative note).
See an example DocumentReference that illustrates this guidance.
The Prescriber Intermediary server application sits in between the EHR system and the REMS Administrator. The benefit to this is allowing the REMS Administrator system to register their CDS Hooks with any supported intermediaries instead of every EHR system. The CDS Hooks requests are sent to the Prescriber Intermediary when configured to do so. This intermediary will determine based on the medication in the hook which REMS Administrator to send the request to. The intermediary will then forward back any returned cards from the REMS Administrator to the EHR. The interaction will be transparent to the EHR system. The intermediary SHALL populate the prefetch if unset using the prefetch tokens provided by the REMS Administrator. Lastly, the intermediary SHALL remove the FHIR Authorization from the Hook before sending it to the REMS Administrator.

The Prescriber Intermediary SHOULD also support forwarding FHIR requests from the EHR to the REMS Administrators. Similarly to the CDS Hooks requests, FHIR requests will be forwarded. This enables the $rems-etasu FHIR operation (for retrieving the ETASU out-of-band) and the $questionnaire-package operation (for retrieving Questionnaires in a shared SMART on FHIR application scenario).
Similar to the burden with registering the CDS Hooks server on the REMS Administrator with every EHR, there is significant effort during setup to register the SMART on FHIR application from the REMS Administrator with every EHR. The REMS Administrators have the option to implement their own SMART on FHIR application that may give them tighter control, however REMS Administrators SHOULD support shared SMART App launch instead. The Shared SMART app SHALL follow selected portions of the SMART on FHIR application guidance in Da Vinci Documentation Templates and Rules (DTR) IG. These sections include retrieving forms from the server, pre-population, loading and saving partially completed forms, and submitting forms upon completion. Optional elements include Adaptive Forms and support for EHR native applications. Strict adherence to the entire DTR IG is not necessary but enough SHOULD be supported for greater interoperability.
The shared SMART app SHALL request the resources necessary to render the forms from the REMS Administrators using the $questionnaire-package operation on the Questionnaire resource. The path to the operation on the REMS Administrator’s FHIR server will follow the pattern <fhir_server_base>/Questionnaire/<questionnaire-id>/$questionaire-package. When retrieving the questionnaire package, the REMS Administrator will compile a FHIR bundle containing the Questionnaire, ValueSet, and any Library resource needed to render the form. Embedded within Library resources there SHOULD be CQL (Clinical Quality Language) expressions. These expressions link the Questionnaire to data within the FHIR server. Once executed by the Shared SMART App, they are able to pre-populate the forms with data. Without the CQL, the forms will be empty when loading, negating the potential benefit of using a SMART on FHIR application.
While the forms are being completed, the data SHALL be stored within a QuestionnaireResponse FHIR resource. The application SHOULD provide a method for storing and retrieving in-progress forms from the EHR FHIR server. This storage and retrieval method SHALL be implemented using standard storage and retrieval methods for QuestionnaireResponse resources on the FHIR server. The shared application SHOULD query for all QuestionnaireResponses for this combination of Patient and medication and give the user completing the form the option to select which they would like to continue. The shared SMART on FHIR application SHALL render the partially completed form with the answers already provided in the stored and loaded QuestionnaireResponse.
Upon completion of the form, the application SHALL send the QuestionnaireResponse to the correct REMS Administrator for the medication. The application MAY send the responses through the Prescriber Intermediary, or directly to the REMS Administrator. The REMS Administrator SHALL support a FHIR Operation $submit on the QuestionnaireResponse resource. The path will follow the pattern <base_fhir_url>/QuestionnaireResponse/$submit. The REMS Administrator is then free to parse and store the QuestionnaireResponse following the requirements of the REMS program.
This Implementation Guide is part of a larger system whose scope encompasses not just the Patient and Provider interactions with the REMS Administrator, but also interactions with the Pharmacy. The full system completes the interaction from the initial Provider/Patient interaction to the final Pharmacy/Patient interaction. This starts with the Provider meeting with a Patient and determining that a medication is needed that has a REMS. Through the technologies outlined in this guide they are able to determine what the requirements are for the REMS program and complete those before sending the medication prescription on to the Pharmacy. Once the prescription is sent to a Pharmacy, the REMS interactions are not complete until the medication is dispensed to the patient. In fact, there may even be further interactions with the Provider that check the status of the Patient and determine that the benefits of the Patient using the medication still outweigh the risks.

The Pharmacy interactions are out of scope of this IG but are detailed in the NCPDP Implementation Guides (see the NCPDP standards page for more information). These interactions detail the use of the REMS specific messages within the NCPDP SCRIPT standard. Using the standard, the Pharmacy system is able to use standard messages to query the REMS Administrator though a REMS Pharmacy Intermediary. This intermediary forwards the messages to the correct REMS Administrator and returns reject codes if the medication cannot be dispensed. A successful message will provide dispense authorization for the Pharmacy to finally dispense the medication to the Patient.
The EHR SHALL send the medication to the Pharmacy using the standard NCPDP SCRIPT NewRx message. This message contains information about the Patient and the Medication being prescribed. For more details on the message please see the NCPDP SCRIPT specification. Under current prescribing processes, the NCPDP SCRIPT NewRx message is sent from the EHR to an eScript intermediary and then is routed to the correct pharmacy as depicted in the figure above.
The message also contains a tagged value called REMSAuthorizationNumber. This value SHALL contain the REMS Case Number for the given Patient and Medication. This case number SHOULD have been previously retrieved from the REMS Administrator though the $rems-etasu FHIR Operation described below. If there is no case number available, the REMSAuthorizationNumber can be omitted.
A REMS Administrator may not create a case number for the Patient until enrollment or other forms have been completed. The case number is used to reference the case and make it easier for the case to be retrieved by the REMS Administrator internally without having to rely on Patient demographics or other Patient matching algorithms.
This guide does not build a specific mechanism for sending a message back from the Pharmacy to the EHR. Existing methods should be utilized for notifying the Provider that REMS requirements still need to be completed before the medication can be dispensed. Future versions of this guide may outline the details surrounding new communication mechanisms to automate this interaction.
The REMS Administrator will typically need information about the patient, provider and drug to support a REMS interaction, regardless of the REMS program or point in the patient’s care.
But individual programs may require sharing additional patient clinicals or other info with the REMS Administrator as part of the Hooks interaction so that it can determine how best to respond.
Supplying a consistent set of FHIR resources in the CDS Hooks request is needed to provide sufficient context to enable the REMS Administrator to respond–regardless of the medication or situation.
The Provider System SHOULD support include the following FHIR resources as prefetch data within CDS Hooks requests submitted to a REMS Administrator’s CDS service. The REMS Administrator’s CDS service SHALL query the Provider System to retrieve the resources below if not provided in the CDS request.
For example:
{
...
"prefetch" : {
"patient": "Patient/{{context.patientId}}",
"practitioner": "{{context.userId}}",
"medicationRequests": "MedicationRequest?subject={{context.patientId}}&_include=MedicationRequest:medication"
}
}Provider Systems SHALL enable the REMS Administrator to query for additional patient clinical or other information during the CDS exchange, for example to retrieve lab results or other diagnostics specific to a REMS drug program
There may be instances where a client to the REMS Administrator may need information about the current ETASU (Elements to Assure Safe Use) status of the REMS program. A new FHIR operation $rems-etasu on the GuidanceResponse resource SHALL be supported by the REMS Administrator FHIR Server. The path for this operation will follow the pattern <base_fhir_url>/GuidanceResponse/$rems-etasu. The operation allows the clients to the REMS Administrator FHIR server to query the status of the REMS process for an individual patient at any time. The Provider and the Pharmacy Systems MAY query the REMS Administrator FHIR Server using the $rems-etasu operation. The users of these may include the Patient, Provider, or Pharmacist. The operation will also return the case number if available for the REMS case associated with the Patient and Medication that are provided as input Parameters. This operation allows for the systems to programmatically check the ETASU status in a parsable output format that could then be displayed to the users in a graphical and more user-friendly method. The data can also be used to determine the case number for use when sending the prescription to the Pharmacy using the NewRx NCPDP SCRIPT message.
The input parameters optionally consist of a Patient and Medication FHIR Resource or a case number. These resources are used by the REMS Administrator to retrieve the REMS case for the provided patient.
{
"resourceType": "Parameters",
"parameter": [
{
"name": "patient",
"resource": {
"resourceType": "Patient",
"id": "example-patient-123",
"meta": {
"versionId": "1",
"lastUpdated": "2024-03-27T12:19:51.575-04:00",
"source": "#rHsFtpinBxvVskjP"
},
"text": {
"status": "generated",
"div": "<div xmlns=\"http://www.w3.org/1999/xhtml\">…</div>"
},
"identifier": [
{
"system": "http://hl7.org/fhir/sid/us-medicare",
"value": "0V843229061TB"
}
],
"name": [
{
"use": "official",
"family": "Samuels",
"given": [
"August",
]
}
],
"gender": "male",
"birthDate": "1989-03-12",
"address": [
{
"use": "home",
"type": "both",
"line": [
"10023 Oakways Ln"
],
"city": "Concord",
"state": "MA",
"postalCode": "01742"
}
]
}
},
{
"name": "medication",
"resource": {
"resourceType": "Medication",
"id": "123-mr-IPledge-med",
"code": {
"coding": [
{
"system": "http://www.nlm.nih.gov/research/umls/rxnorm",
"code": "6064",
"display": "Isotretinoin 20 MG Oral Capsule"
},
{
"system": "http://hl7.org/fhir/sid/ndc",
"code": "0245-0571-01"
}
]
}
}
},
{
"name": "case_number",
"valueString": "a24e73e53b2"
}
]
}
The output consists of a FHIR Parameter with a FHIR Resource of the type GuidanceResponse. The GuidanceResponse contains a status value mapped to the REMS ETASU status in the following table.
| GuidanceResponse Status | REMS ETASU Status |
|---|---|
| success | Completed |
| data-requested | |
| data-required | Incomplete / Needed |
| in-progress | |
| failure | Not Found |
| entered-in-error |
This GuidanceResponse represents the overall status of the REMS ETASU. Inside the GuidanceResponse there is a contained Parameters list that is referenced by the outputParameters field. Each parameter in this list contains a GuidanceResponse resource that is representative of one of the individual elements of the REMS program. These may include any forms or knowledge assessments that need to be completed. The status of the GuidanceResponse gives the completion status of the REMS ETASU requirement. The values are mapped in the table above.
{
"resourceType": "Parameters",
"parameter": [
{
"name": "rems-etasu",
"resource": {
"resourceType": "GuidanceResponse",
"status": "data-required",
"moduleUri": "https://build.fhir.org/ig/HL7/fhir-medication-rems-ig/",
"subject": {
"reference": "Patient/example-patient-123"
},
"outputParameters": {
"reference": "#etasuOutputParameters"
},
"contained": [
{
"resourceType": "Parameters",
"id": "etasuOutputParameters",
"parameter": [
{
"name": "Patient Enrollment",
"resource": {
"resourceType": "GuidanceResponse",
"status": "success",
"moduleUri": "https://build.fhir.org/ig/HL7/fhir-medication-rems-ig/",
"subject": {
"reference": "Patient/example-patient-123"
},
"note": [
{
"text": "Patient Enrollment"
}
]
}
},
{
"name": "Prescriber Enrollment",
"resource": {
"resourceType": "GuidanceResponse",
"status": "data-required",
"moduleUri": "https://build.fhir.org/ig/HL7/fhir-medication-rems-ig/",
"subject": {
"reference": "Patient/example-patient-123"
},
"note": [
{
"text": "Prescriber Enrollment"
}
]
}
},
{
"name": "case_number",
"valueString": "a24e73e53b2"
}
]
}
]
}
}
]
}
The use of a REMS Prescriber Intermediary server sitting between the EHR and the REMS Administrator allows for the EHR to only register a single CDS Hooks endpoint. The burden of registering all the REMS Administrators is shifted to a more centralized point within the REMS Prescriber Intermediaries. This burden can be further reduced by allowing the REMS Prescriber Intermediary to automatically discover and register the CDS Hooks endpoints provided by the REMS Administrators for each REMS program. The combined capabilities of a recommended API similar to the openFDA API and recommended use of REMS Structured Product Labeling (SPL) could enable the automated discovery of the REMS Administrator endpoints in a sustainable manner over time.
Structured Product Labeling (SPL) is a document markup standard approved by Health Level Seven (HL7) and adopted by FDA as a mechanism for exchanging product and facility information. The REMS document and appended materials are also required to be submitted to the FDA using the SPL format. This includes details on the requirements for the REMS program and specifies all forms and Elements to Assure Safe Use (ETASU) requirements. The SPL format also allows for storing REMS Electronic Resource Information. The REMS Electronic Resource Information can be in the format of a URL (Uniform Resource Locator) or URN (Uniform Resource Name).
If an SPL file includes the URL of the CDS Hook that connects the prescriber EHR to the REMS Administrator, the entire zip file from DailyMed’s SPL Resources: Download ALL Indexing & REMS Files webpage containing the REMS SPL files can be downloaded and parsed for those CDS Hook endpoint URLs. The REMS Administrator CDS Hook URLs can then be discovered, registered, and accessed by the REMS Prescriber Intermediary to route the request to the correct REMS Administrator based upon the REMS drug ordered by the prescriber.
The FDA provides the openFDA Application Programming Interface (API) for querying drug product labeling information. The results from these queries are returned in JSON format. Detailed information about the openFDA API can be found at https://open.fda.gov/apis/. For guidance on using the drug labeling endpoint, one can visit “How to Use the Endpoint” at https://open.fda.gov/apis/drug/label/how-to-use-the-endpoint/. The openFDA API includes endpoints for packaged product National Drug Codes (NDCs) to query specific medication data, including naming information, ingredient information, and packaging information amongst others.
A recommended API similar to the openFDA API could provide expanded results for REMS drugs that include REMS Administrator and REMS endpoint information. If REMS endpoint information is provided for the CDS Hook URLs, they can be discovered, registered, and accessed by the REMS Prescriber Intermediary to route the request to the correct REMS Administrator based upon the REMS drug ordered by the prescriber.
If an SPL file includes the URL of the CDS Hook that connects the prescriber EHR to the REMS Administrator, the endpoint information can be pulled from the DailyMed’s SPL Resources: Download ALL Indexing & REMS Files webpage or from some other resource that consistently provides the submitted REMS SPL files.
To understand the construction of the reference value URN, the below is an example of the REMS Electronic Resource Information embedded in the SPL in the following format:
<subjectOf>
<document>
<id root="00000000-0000-0000-0000-000000000006"/>
<title>REMS SPL Pilot – NCPDP D0 - Patient Data </title>
<text>
<reference value="urn:NCPDP:D.0:P1:610674:00000000-0000-0000-0000-000000000005"/>
</text>
</document>
</subjectOf>
The reference value contains a URN with the following components:
Below is an example of how this reference value might be constructed for a FHIR CDS Hooks service:
<reference value="urn:HL7:FHIR4.0:rems_cds_discovery:cdshooksserver.remsdrug.com/cds-services" />. In this case, the components of the URN are as follows:
The example above lists the “rems_cds_discovery” endpoint as “cdshoooksserver.remsdrug.com/cds-services”. This URL within the URN can be used to reference the CDS Hooks server. The REMS Prescriber Intermediary can query this endpoint with a metadata request for the CapabilityStatement to find all the supported endpoints and capabilities and confirm that the capabilities match those required as described in the CodeX US Medication REMS FHIR IG.
Below is an example of how this reference value might be constructed for a FHIR Server base url: <reference value="urn:HL7:FHIR4.0:rems_fhir_base:fhirserver.remsdrug.com/fhir/" />
In this case, the components of the URN are as follows:
The example above lists the “rems_fhir_base” endpoint as “fhirserver.remsdrug.com/fhir”. This URL within the URN can be used to reference the base url for the FHIR server. From this base url all FHIR queries can be completed. This base url can be used by the intermediary for forwarding requests to the $rems-etasu and $questionnaire-package operations.
In addition to the REMS Document in SPL, a recommended API similar to the the openFDA API may provide the URL for the REMS Administrator CDS Hooks endpoint. This would in turn be readable by the REMS Prescriber Intermediary allowing for automatic registration of the REMS Administrator Endpoints.
Like the openFDA API, the data elements available include the Generic Name, Brand Name, and packaged product NDC, all of which are queryable elements within this API. Additionally, the recommended API would include data elements for REMS Administrator API Endpoint, REMS Administrator, REMS Approval Date, and REMS Modification Date. A client can search for REMS medication information based on one of the three queriable data element values. The package-specific NDC is most specific and reflective of the codes that will be used in a real-world environment. The REMS Administrator API Endpoint data element (rems_endpoint) contains the URL of the REMS Administrator CDS Hooks endpoint for the queried medication. If there is no endpoint supplied, there may be no CDS Hooks endpoint available for the REMS Administrator yet.
When queried for the Turalio medication, the following is an example output showing the recommended REMS data elements:
{
"meta": {
"disclaimer": "disclaimer",
"terms": "terms",
"license": "license",
"last_updated": "2025-03-13",
"results": {
"skip": 0,
"limit": 1,
"total": 1
}
},
"results": [
{
"brand_name": "Turalio",
"generic_name": "PEXIDARTINIB HYDROCHLORIDE",
"product_ndc": "65597-407",
"rems_administrator": "REMS Prototype",
"rems_endpoint": "http://cdshoooksserver.remsdrug.com/cds-services/",
"rems_approval_date": "20240906",
"rems_modification_date": "20240906",
"packaging": [
{
"package_ndc": "65597-407-20",
"description": "1 BOTTLE in 1 CARTON (65597-407-20) / 120 CAPSULE in 1 BOTTLE",
"marketing_start_date": "20230201",
"sample": false
}
]
}
]
}
FHIR Server endpoints for the REMS Administrator are recommended for operations such as the out-of-band ETASU check. A second endpoint in the REMS Prescriber Intermediary should be maintained pointing to the REMS Administrator’s FHIR server. This endpoint can be discovered using the methods outlined above but labelled as “fhir_server” instead of “rems_endpoint”.
The REMS Prescriber Intermediary can periodically retrieve the REMS SPL zip archive to find new REMS medications and their respective CDS Hooks and FHIR server endpoints. This operation could happen on a specific interval, or with a trigger such as being notified when the SPL archive has been updated. The REMS Prescriber Intermediary can also query the recommended API for newer CDS Hooks and FHIR server endpoints based on the drug packaged product NDC code.
Implementers are expected to…
follow core FHIR security principles.
protect patient privacy as described in FHIR Security and Privacy Considerations.
Provider Systems and REMS Administrators SHALL follow guidance defined in…
The Prescriber Intermediary is useful for forwarding CDS Hooks requests from the EHR to the correct REMS Administrator. Passing the FHIR authorization on to a third party that was not registered with the EHR is disallowed. Therefore, the FHIR authorization SHALL be stripped from the hook request before being forwarded to the REMS Administrator. This can leave a problem with the prefetch not properly being populated. In this case, the intermediary SHALL populate the prefetch using the FHIR authorization that it had stripped from the hook. This will provide all needed information to the REMS Administrator in order to process the hook request without sharing authorization beyond its intended scope.