Electronic Long-Term Services and Supports (eLTSS) Release 1 - US Realm, published by HL7 International / Human and Social Services. This guide is not an authorized publication; it is the continuous build for version 2.0.0 built by the FHIR (HL7® FHIR® Standard) CI Build. This version is based on the current content of https://github.com/HL7/eLTSS/ and changes regularly. See the Directory of published versions
Contents:
LTSS is currently a document-oriented exchange paradigm (i.e., consumers exchange the entire service plan as a document), however during outreach stakeholders expressed an interest in the ability to exchange portions of service plan data, query specific elements, receive notifications, etc. The aim of eLTSS is to enable those exchanges and features for LTSS data.
During the eLTSS Initiative, two user stories were developed and documented into the use case document:
The first user story would use FHIR Resources to generate an eLTSS plan in an LTSS case management system. The set of FHIR Resources to represent the eLTSS Dataset elements could include: Bundle, CarePlan, Claim, Condition, Contract, Coverage, DocumentReference, Encounter, EpisodeOfCare, Goal, Location, Observation, Organization, Patient, Practitioner, Questionnaire, QuestionnaireResponse, Related Person, RiskAssesment, ServiceRequest
Once an eLTSS plan is created using FHIR, there are 4 sample use cases that highlight the possible exchanges that an eLTSS Plan may be involved in (user story 2 above). The figure below illustrates these use cases.
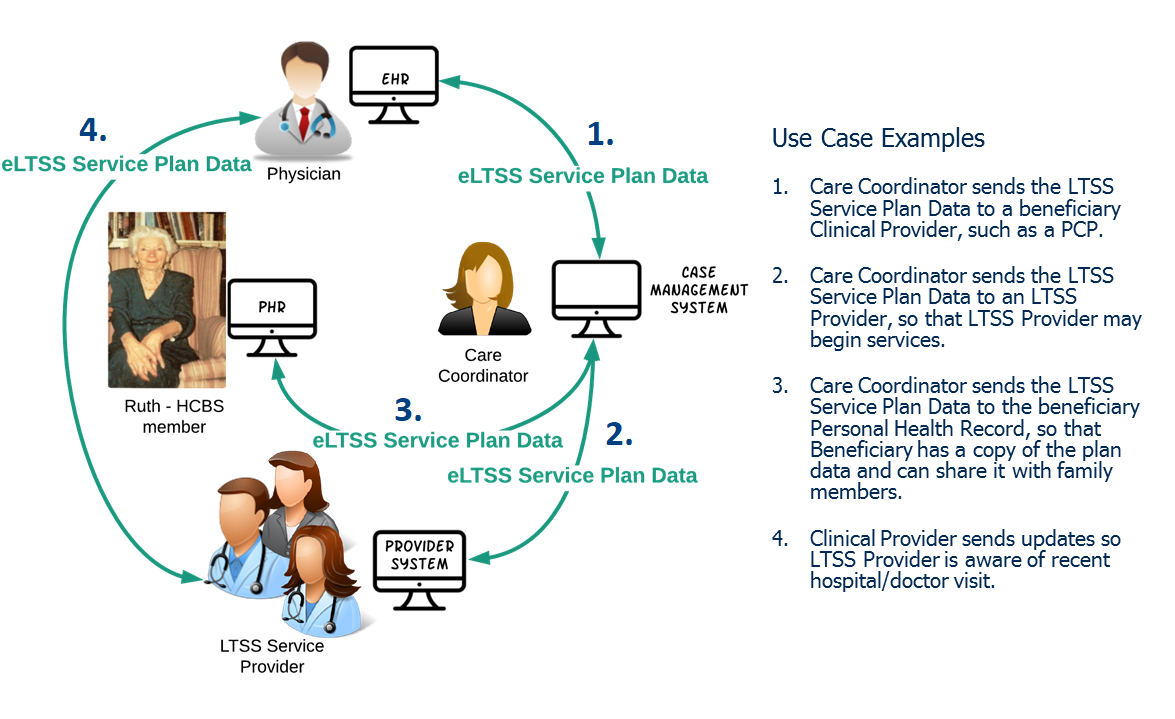
Purpose: The clinical and institutional-based provider is informed of what service(s) the patient/care recipient is eligible for and to supply additional details around the services as well as the patient/care recipient to enable better delivery of services and support.
eLTSS Data: Clinical and Institutional-based Provider may need cost information (Claim), emergency backup plan (CarePlan), full details on service quantities (ServiceRequest), etc. Important information includes contact information for a financial management worker (Practitioner).
Purpose: To inform HCBS Provider of service(s) requested by patient/care recipient, or are authorized for the patient/care recipient, as well as to supply additional detail around those services and the patient/care recipient to enable better delivery of services and supports.
eLTSS Data: HCBS Providers may need service and cost information (Units and Unit Costs, Effective Dates, etc.) (ServiceRequest, Claim), especially if there is a change (e.g., due to a re-assessment). This use case could be the vehicle to communicate these data elements to the HCBS Providers officially, even if the services (and quantity and rates) were previously negotiated. Signatures (Contract) may not be required; however, the eLTSS Signature Date data elements (Contract) indicating when the plan was approved (CarePlan) could be important.
Purpose: The patient/care recipient has a complete record of what is either proposed or to be provided to them and by whom, and potentially be imported into the patient/care recipient’s PHR.
eLTSS Data: patient/care recipient may not need signatures (Contract) and may not need cost information (Claim).
Purpose: The Clinical Provider is aware of the services the patient/care recipient is receiving and what their goals/needs/risks are or have been. The HCBS Provider is aware of the patient/care recipient's recent hospital/doctor visit and any discharge/treatment instructions to follow.