
This fragment is available on index.html
This publication includes IP covered under the following statements.
| Type | Reference | Content |
|---|---|---|
| web | github.com | Da Vinci Value-Based Performance Reporting Implementation Guide, published by HL7 International / Clinical Quality Information. This guide is not an authorized publication; it is the continuous build for version 1.1.0 built by the FHIR (HL7® FHIR® Standard) CI Build. This version is based on the current content of https://github.com/HL7/davinci-vbpr/ and changes regularly. See the Directory of published versions |
| web | fhir.github.io | Current version of the FHIR Validator |
| web | www.iso.org |
ISO maintains the copyright on the country codes, and controls its use carefully. For further details see the ISO 3166 web page: https://www.iso.org/iso-3166-country-codes.html
Show Usage
|
| web | ucum.org |
The UCUM codes, UCUM table (regardless of format), and UCUM Specification are copyright 1999-2009, Regenstrief Institute, Inc. and the Unified Codes for Units of Measures (UCUM) Organization. All rights reserved. https://ucum.org/trac/wiki/TermsOfUse
Show Usage
|
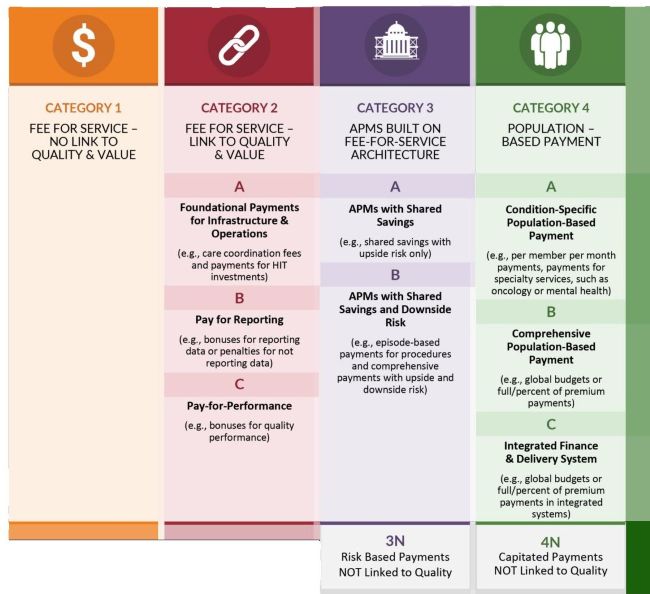
| web | hcp-lan.org | Alternative payment models deviate from traditional fee-for-service (FFS) payment, insofar as they adjust FFS payments to account for performance on cost and quality metrics, or insofar as they use population-based payments that are linked to quality performance. source |
| web | www.acponline.org | A fixed amount of money per patient per unit of time paid in advance to the physician (or health care provider) for the delivery of health care services. The actual amount of money paid is determined by the ranges of services that are provided, the number of patients involved, and the period of time during which the services are provided. source |
| web | www.caqh.org | A set, risk-adjusted dollar amount typically determined by historical fee-for-service spend, market-based trends, or other methods that is used to measure financial performance in VBP Models. Programs using a financial benchmark most closely align with the HCPLAN Categories 3 and 4. (source: CAQH CORE Framework for Semantic Interoperability in Value-based Payments ) |
| web | hcp-lan.org | 1 |
| web | www.rand.org | 1 |
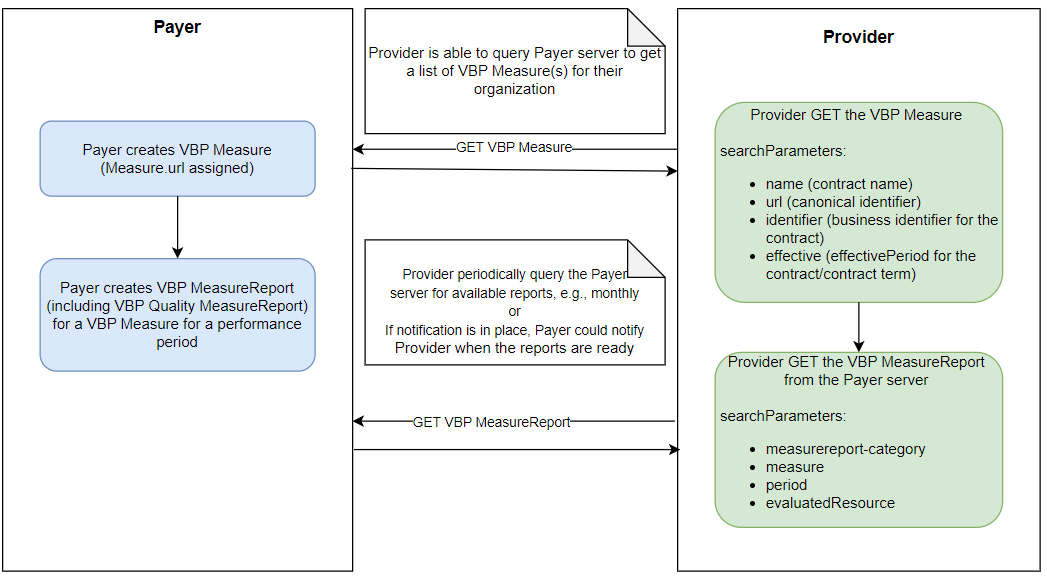
api-workflow.png 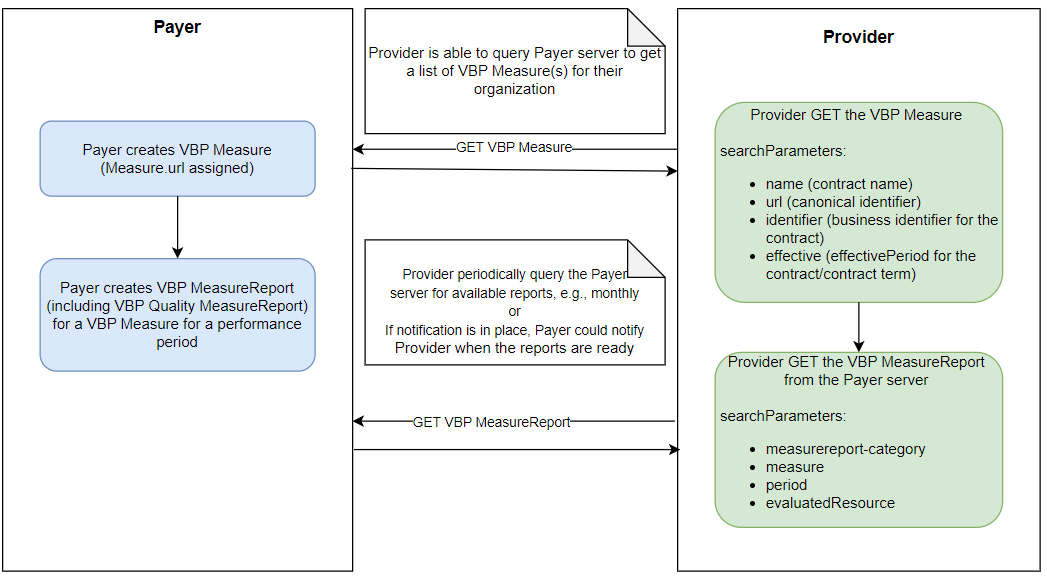
|
hcplan-apm-framework.jpg 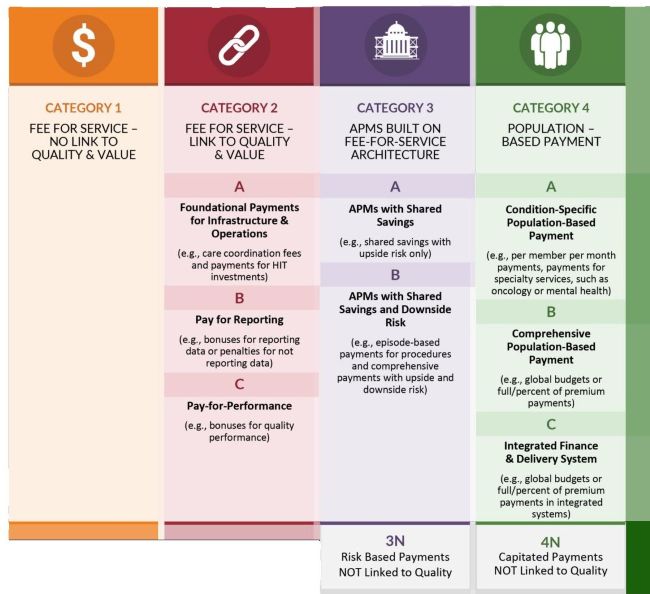
|
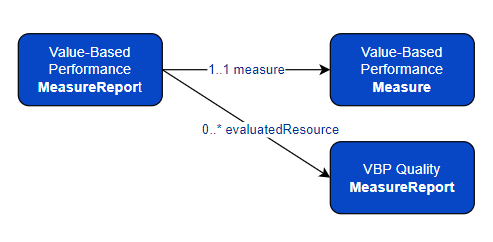
resources.png 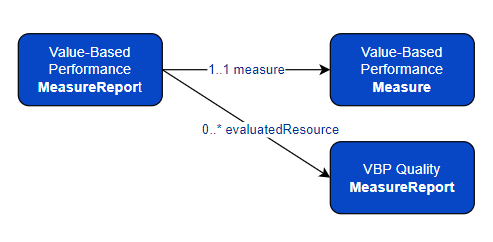
|
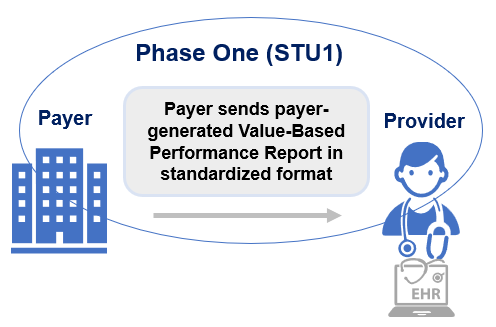
stu1_scope.png 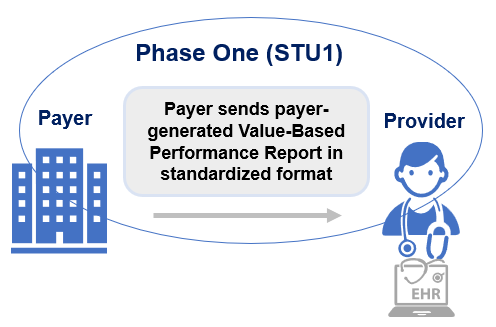
|
tree-filter.png 
|
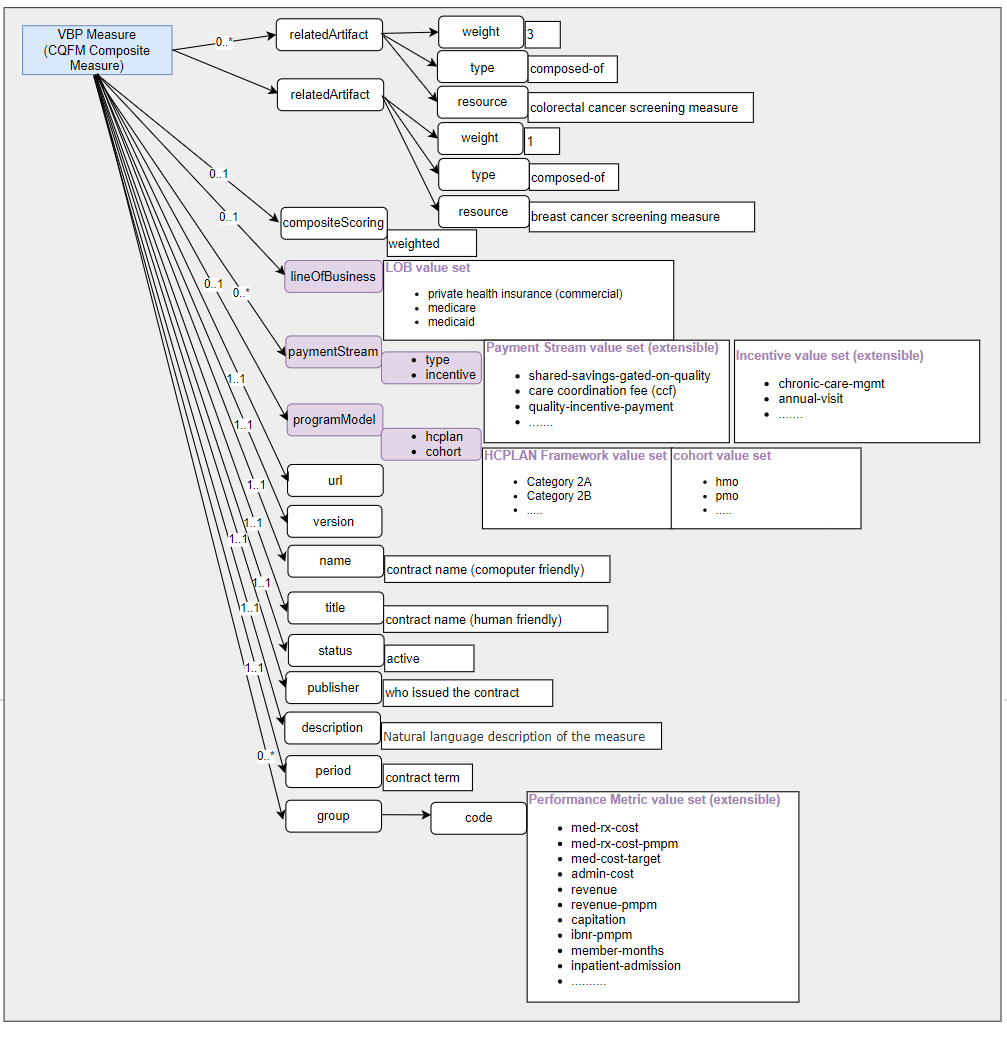
vbp-measure.png 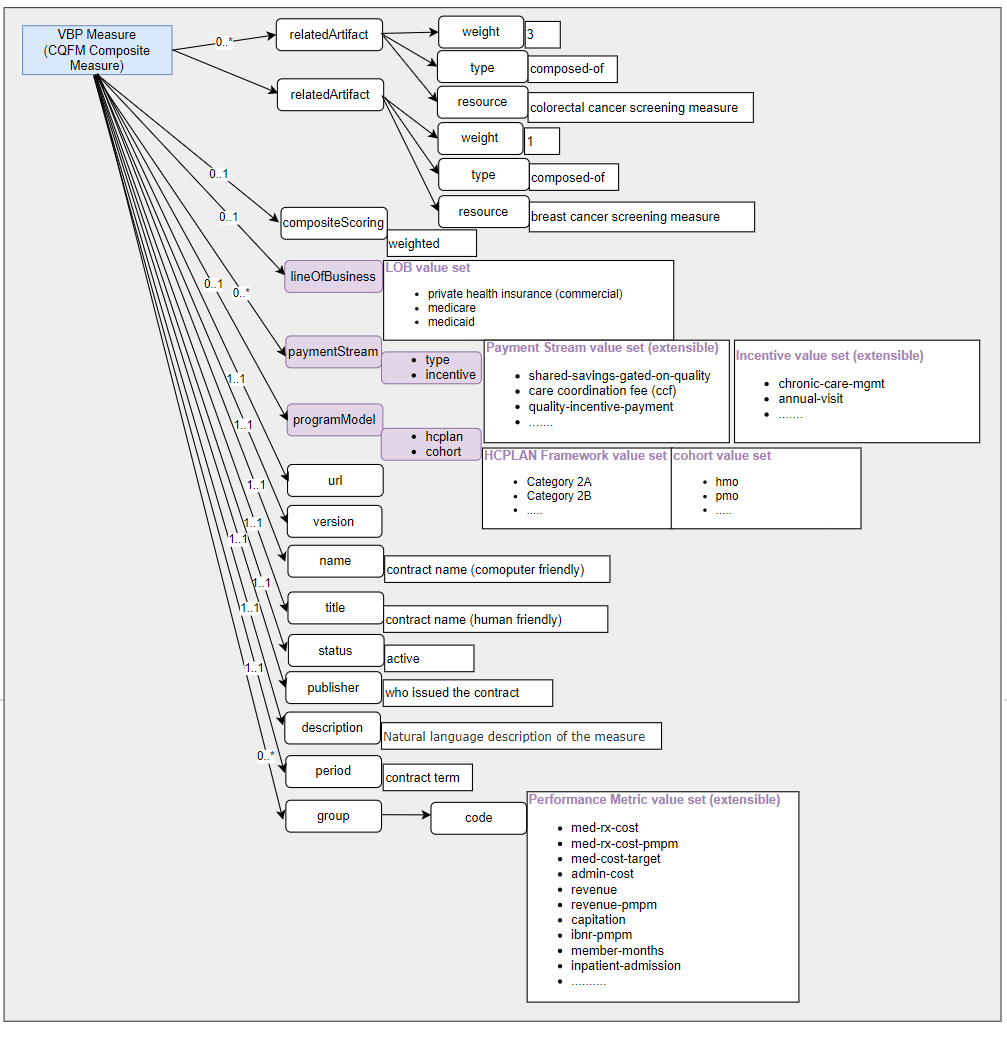
|
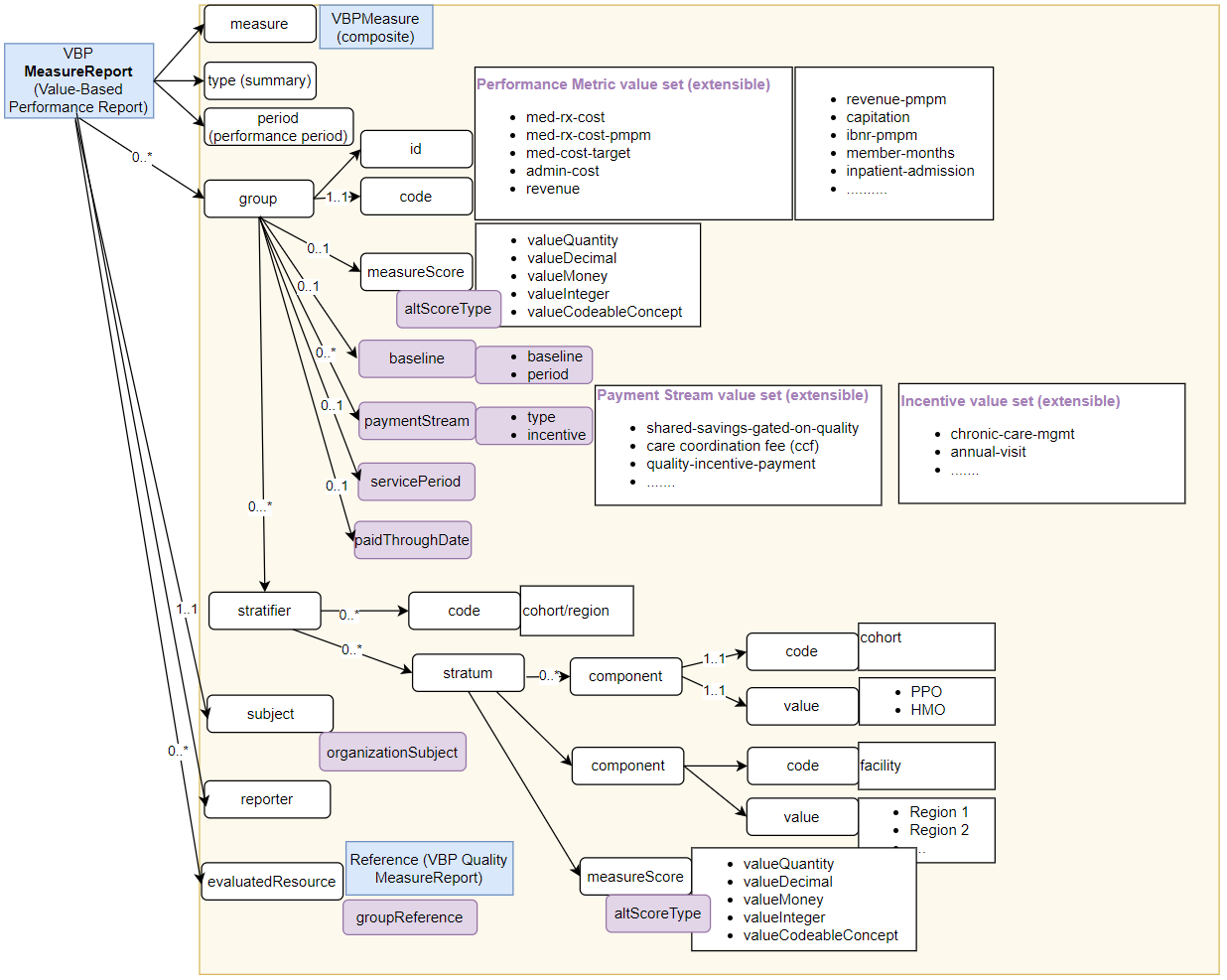
vbp-measurereport.png 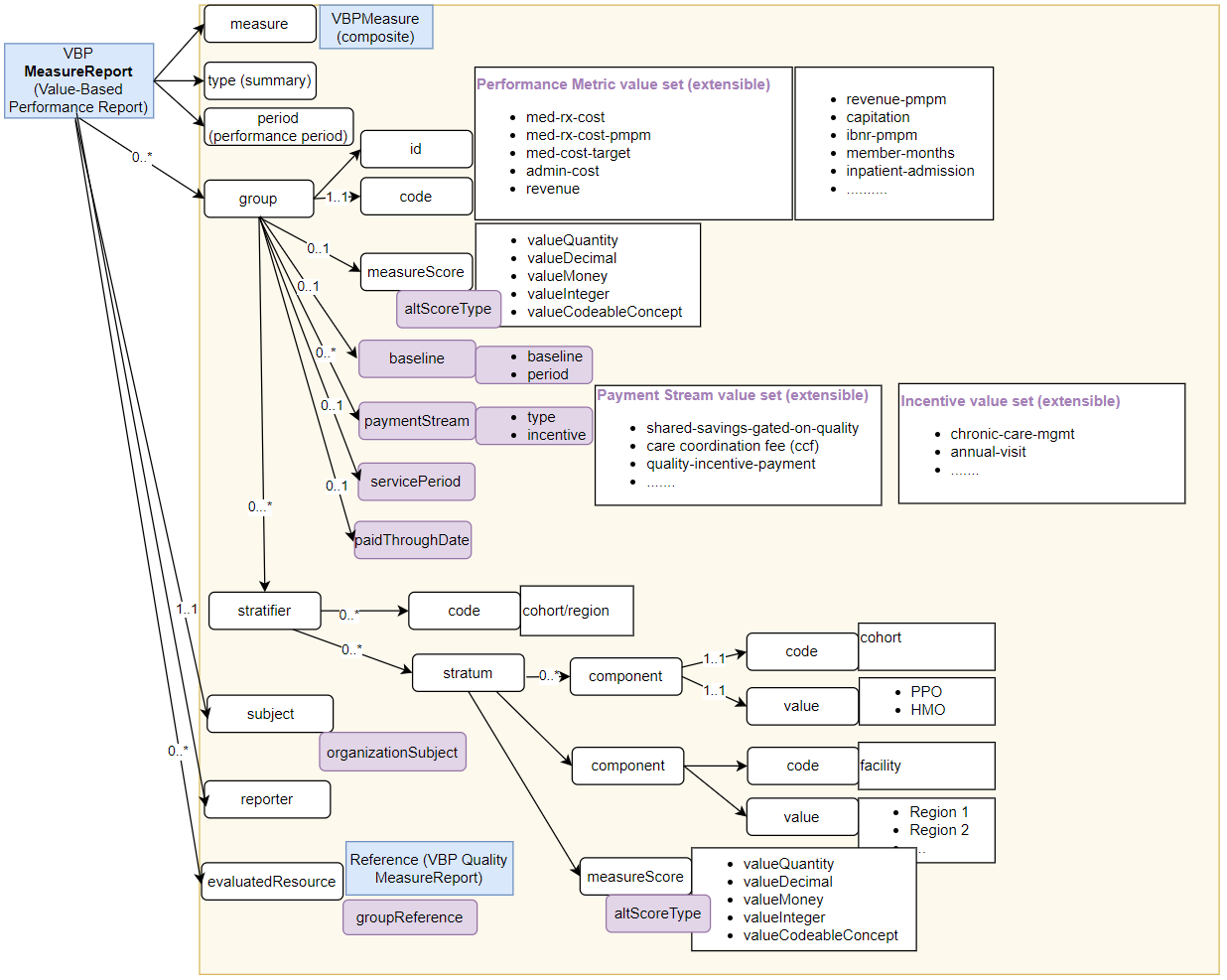
|
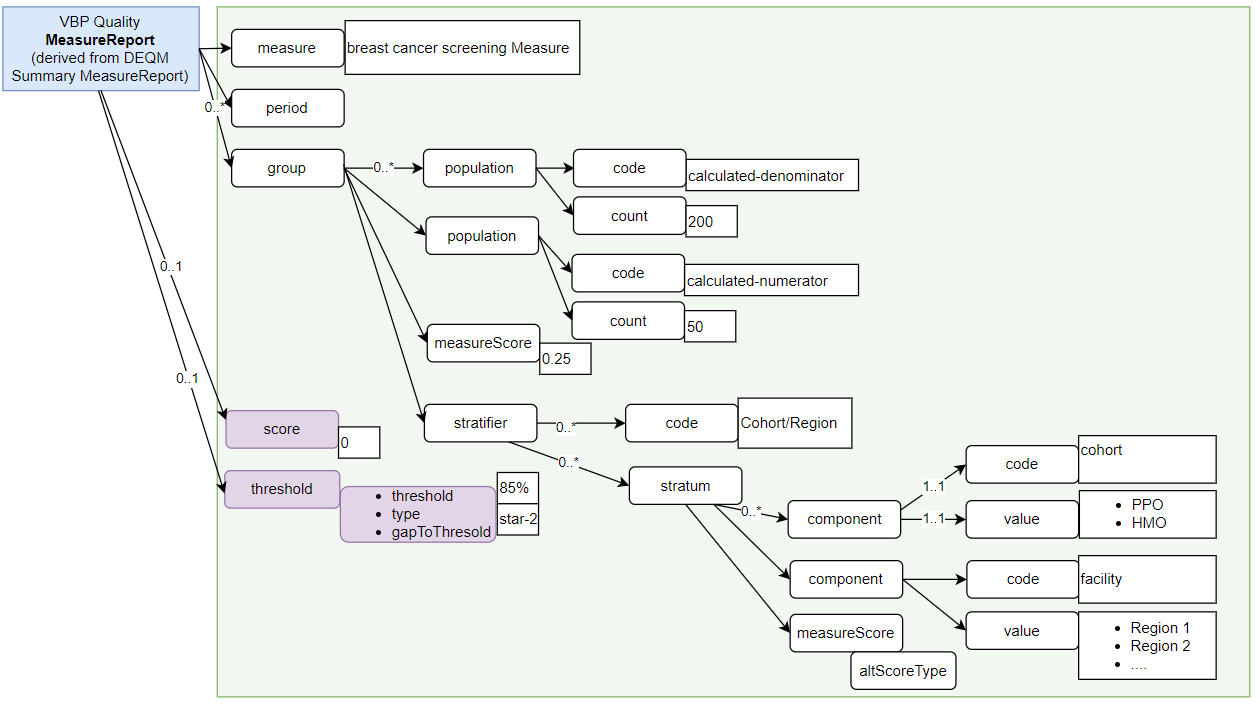
vbp-quality-measurereport-breastcancer.png 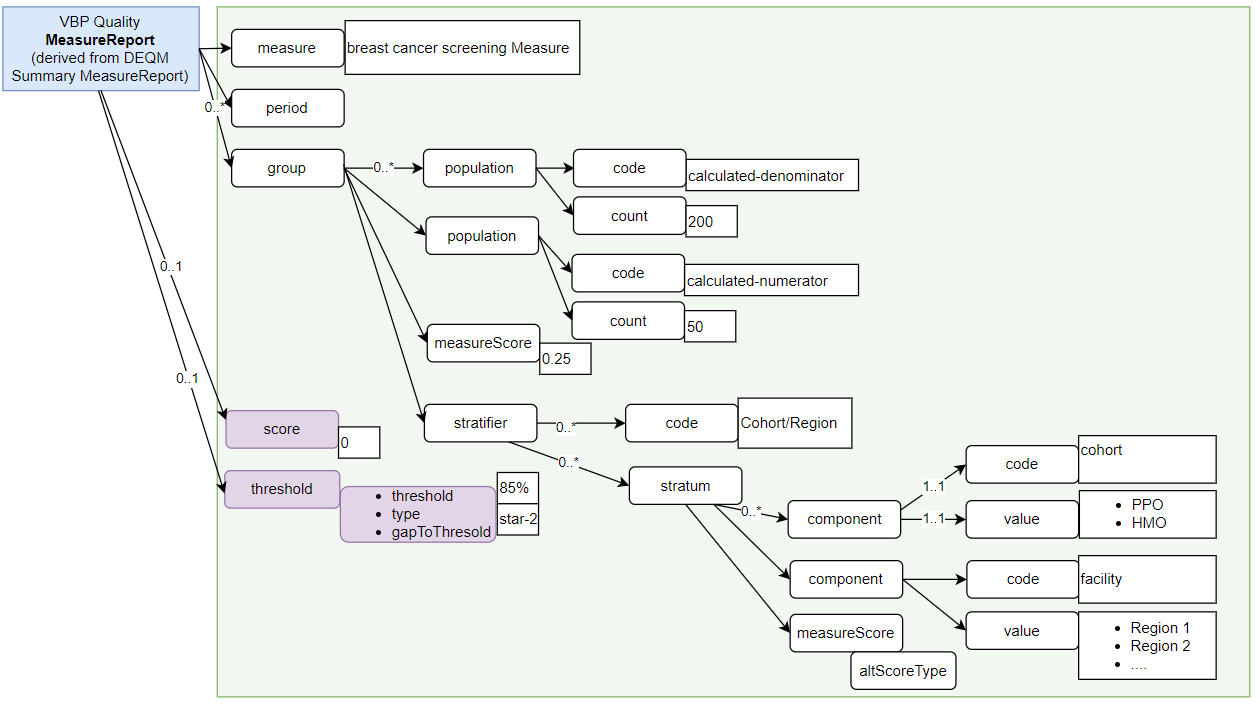
|
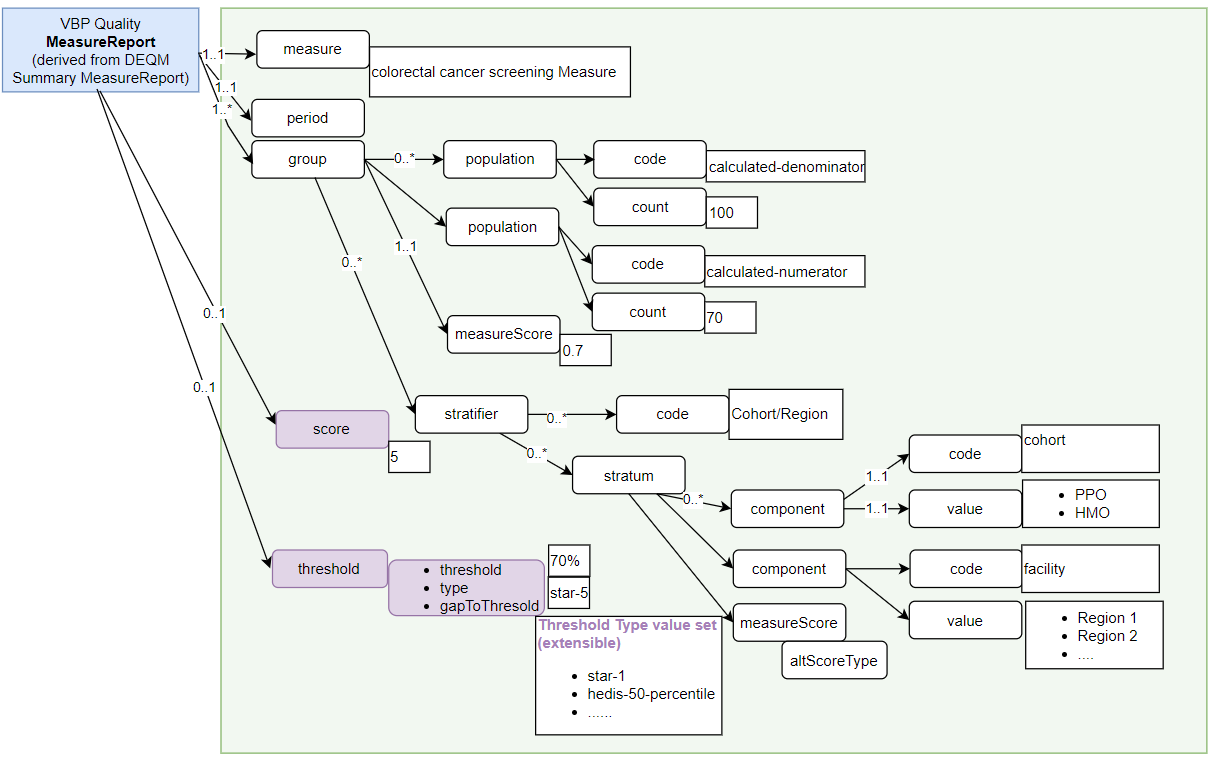
vbp-quality-measurereport-colorectalcancer.png 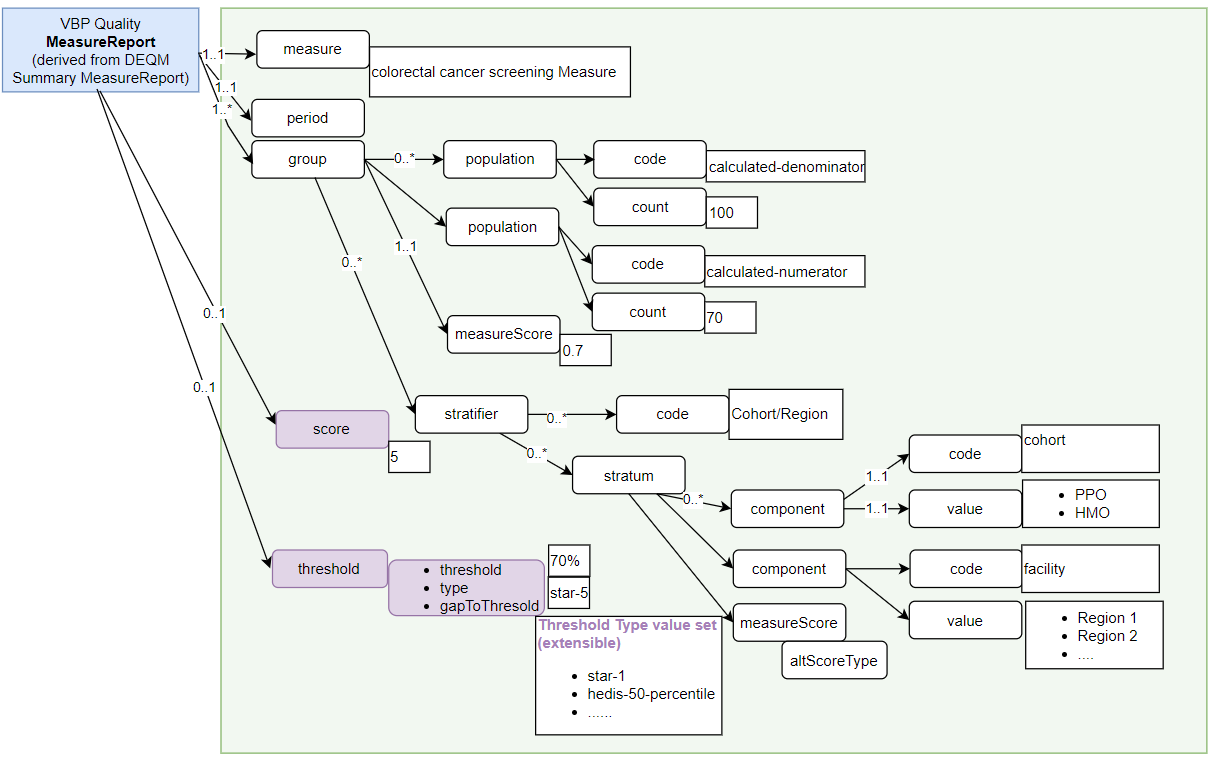
|