2022 CDC Clinical Practice Guideline for Prescribing Opioids Implementation Guide, published by Centers for Disease Control and Prevention (CDC). This guide is not an authorized publication; it is the continuous build for version 2022.1.0 built by the FHIR (HL7® FHIR® Standard) CI Build. This version is based on the current content of https://github.com/cqframework/opioid-cds-r4/ and changes regularly. See the Directory of published versions
Recommendations #4 & #5 (2022 CDC Clinical Practice Guideline for Prescribing Opioids for Pain)
4: When opioids are initiated for opioid-naïve patients with acute, subacute, or chronic
pain, clinicians should prescribe the lowest effective dosage. If opioids are continued for
subacute or chronic pain, clinicians should use caution when prescribing opioids at any
dosage, should carefully evaluate individual benefits and risks when considering increasing
dosage, and should avoid increasing dosage above levels likely to yield diminishing returns in
benefits relative to risks to patients
(recommendation category: A;
evidence type: 3).
5: For patients already receiving opioid therapy, clinicians should carefully weigh
benefits and risks and exercise care when changing opioid dosage. If benefits outweigh risks
of continued opioid therapy, clinicians should work closely with patients to optimize
nonopioid therapies while continuing opioid therapy. If benefits do not outweigh risks of
continued opioid therapy, clinicians should optimize other therapies and work closely with
patients to gradually taper to lower dosages or, if warranted based on the individual
circumstances of the patient, appropriately taper and discontinue opioids. Unless there are
indications of a life-threatening issue such as warning signs of impending overdose (e.g.,
confusion, sedation, or slurred speech), opioid therapy should not be discontinued abruptly,
and clinicians should not rapidly reduce opioid dosages from higher dosages
(recommendation category: B;
evidence type: 4).
Functional Description
- When
- Provider is prescribing an opioid analgesic with ambulatory misuse potential in the outpatient setting
- Opioid review is useful for this patient:
- Patient is 18 or over
- Patient does not have evidence of sickle cell disease
- Patient does not have findings indicating limited life expectancy
- Patient does not have orders for therapies indicating end of life care
- Patient is not undergoing active cancer treatment:
- Patient has had at least 2 office visits within the past 12 months with an oncology specialist present, or
- Patient has had at least 2 office visits within the past 12 months with a CDC malignant cancer condition diagnosis
- Patient does not have conditions likely terminal for opioid prescribing present
- Patient Morphine Milligram Equivalent (MME) greater than or equal to 50
- Then
- Calibrate to Lowest Opioid Dose Needed for Expected Results and Exercise Care When Changing Opioid Dosages:
- Document - Will prescribe a lower dose
- Document - Will calibrate a gradual change in dosage
- Snooze - Benefits outweigh risks, snooze 3 months
- Snooze - Short term benefits outweigh risks, snooze 1 month
- Snooze - N/A add comment, snooze 3 months
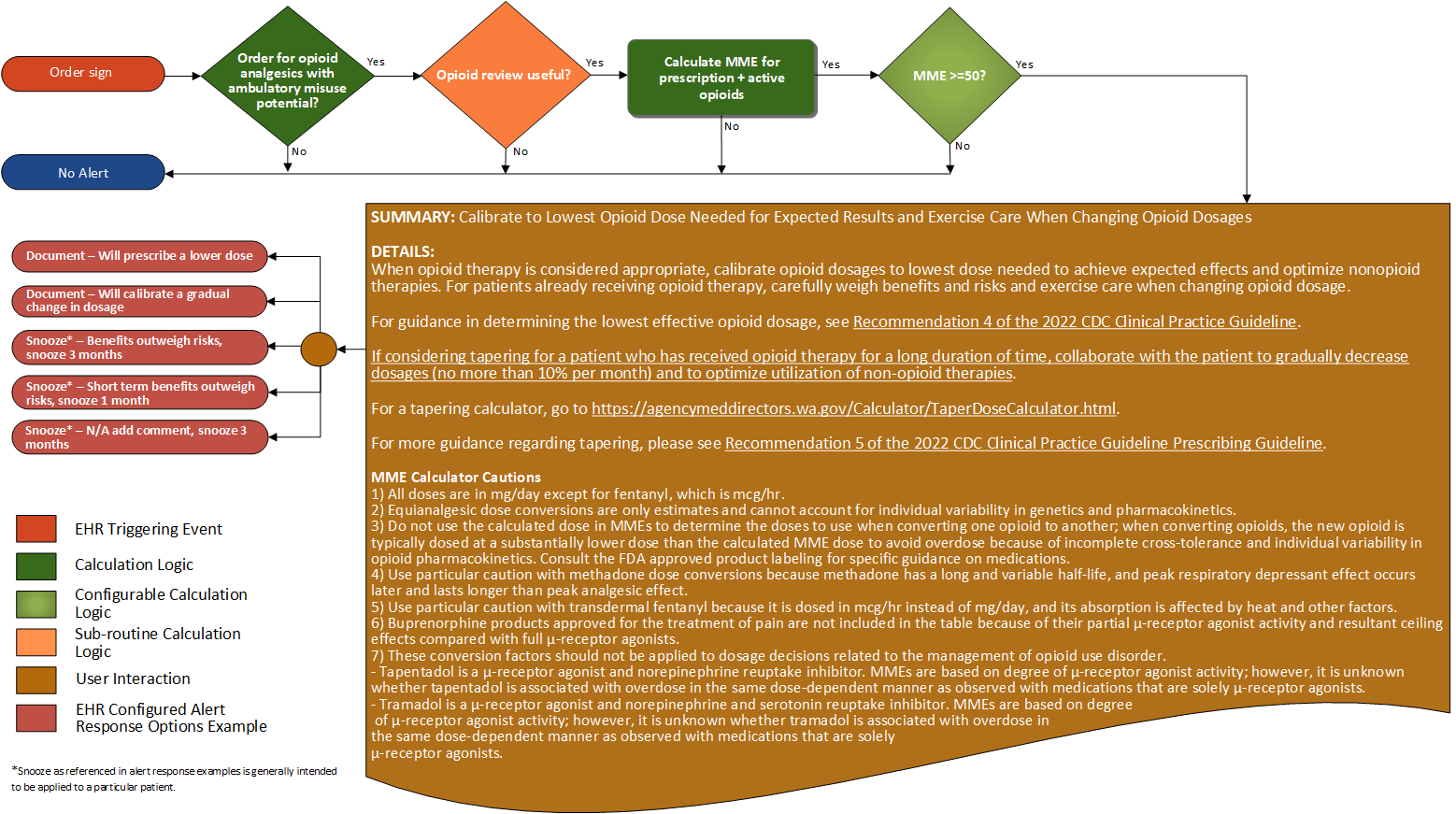
The following table describes the flowchart decisions and sub-routines for the recommendation
| Definition |
Answer to Proceed |
Details |
Data (Terminology) Requirement |
Profile |
Path |
| Order for opioid analgesic with ambulatory misuse potential |
Yes |
Order for opioid analgesics with ambulatory misuse potential |
Opioid analgesics with ambulatory misuse potential |
MedicationRequest
|
MedicationRequest.dispenseRequest.expectedSupplyDuration, MedicationRequest.medication, and MedicationRequest.category
|
| Opioid review useful? |
Yes |
See Opioid Review Useful sub-routine |
|
|
|
| Calculate MME for prescription + active opioids |
N/A |
Current calculation uses known order (prescription) data. Note - for as needed (PRN) medication, the daily
dose assumes the maximum dose the patient may take any given day if a range is present. Ideally, dispensed data
could be used to determine the medication dispensed to the patient |
|
MedicationRequest
|
MedicationRequest.medication.coding.code and MedicationRequest.dosageInstruction
|
| MME≥50? |
Yes |
MME result is ≥ 50 |
|
|
|
Effective Data
Requirements
Opioid Review Useful
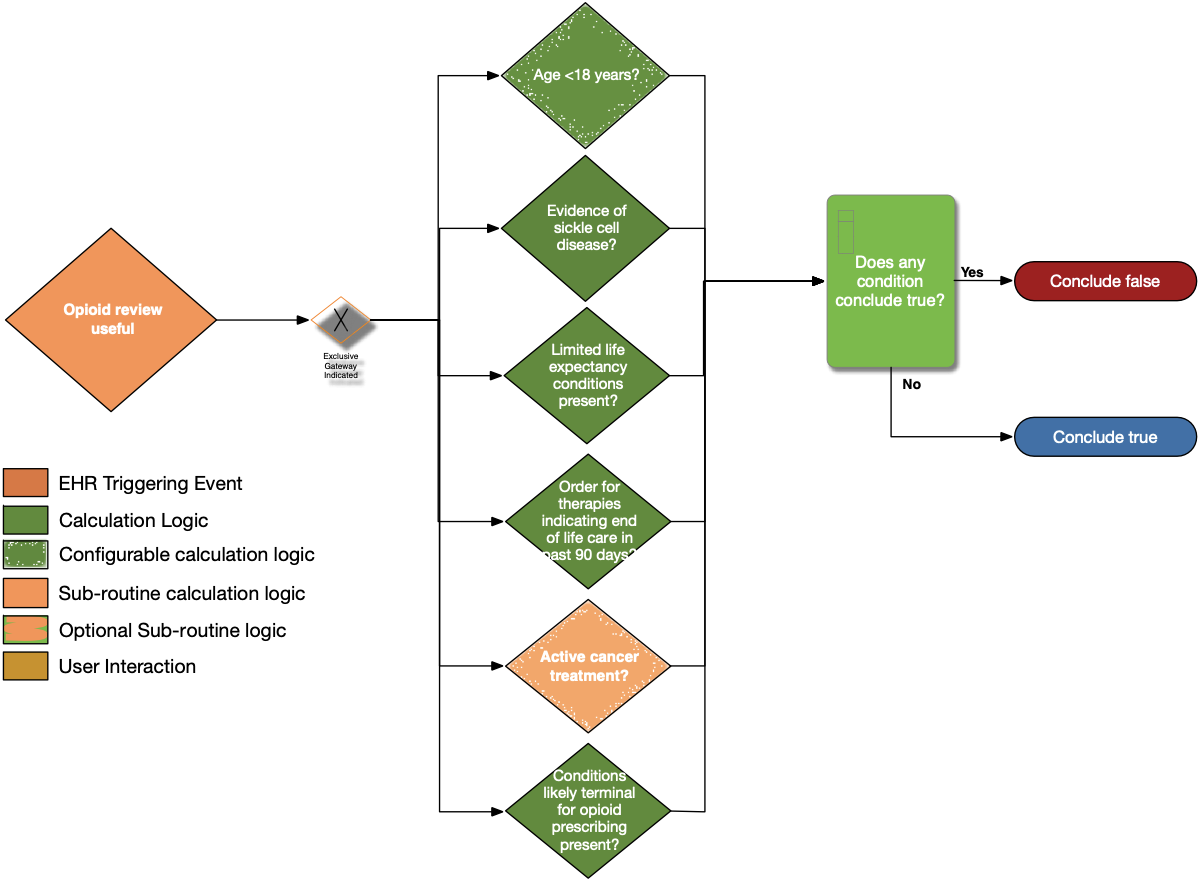
| Definition |
Answer to Proceed |
Details |
Data (Terminology) Requirement |
Profile |
Path |
| Age < 18 years? |
No |
Calculate age from date of birth; exclude patients with age less than 18 years at the time of the prescription |
Date of birth |
Patient |
Patient.birthDate |
| Evidence of sickle cell disease? |
No |
Look for patients with a diagnosis or problem list entry indicating sickle cell disease |
Sickle cell disease condition |
Condition |
Condition.category, Condition.code, and Condition.clinicalStatus |
| Limited life expectancy conditions present? |
No |
Look for documented findings consistent with those listed in the limited life expectancy value set (terminal illness, bad prognosis, pre-terminal) |
Limited life expectancy conditions |
Condition |
Condition.category and Condition.code |
| Order for therapies indicating end of life care in past 90 days? |
No |
Look for patients with an existing order for therapies indicating end of life care written within past 90 days |
Therapies indicating end of life care |
ServiceRequest |
ServiceRequest.status, ServiceRequest.intent, ServiceRequest.authoredOn, and ServiceRequest.code |
| Active cancer treatment? |
No |
See Active Cancer Treatment sub-routine |
See Active Cancer Treatment sub-routine |
|
|
| Conditions Likely Terminal for opioid prescribing present? |
No |
Look for patients with active conditions in the value set end-of-life-conditions |
Conditions likely terminal for opioid prescribing |
Condition |
Condition.category, Condition.code, and Condition.clinicalStatus |
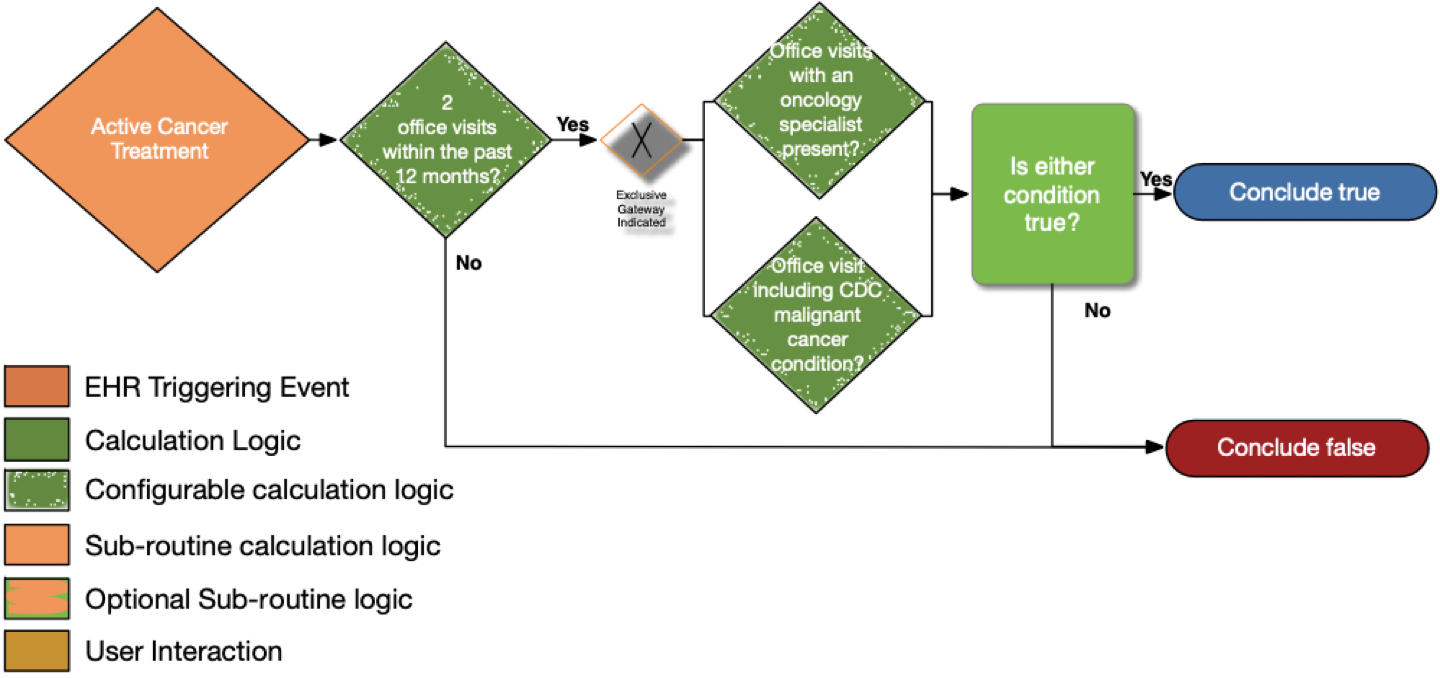
| Definition |
Answer to Proceed |
Details |
Data (Terminology) Requirement |
Profile |
Path |
| Two office visits within the past 12 months? |
No |
Look for a minimum of two distinct encounters within 12 months of the date of the current visit for which each of the following is true:
• the encounter diagnosis (primary or secondary or co-morbidity diagnosis) is listed in the CDC Malignant Cancer Conditions value set |
Office Visit |
Encounter
|
Encounter.class and Encounter.period.start |
| Office visits with an oncology specialist present? |
No |
• The encounter is performed by an oncologist as defined in the oncology specialty designations using the National Uniform Claim
Committee (NUCC) classifications |
Oncology specialty designations (NUCC) |
PractitionerRole and
Encounter
|
PractitionerRole.specialty, Encounter.participant.type, and Encounter.participant.individual |
| Office visits including CDC malignant cancer condition? |
No |
• The encounter diagnosis (primary or secondary or co-morbidity diagnosis) is listed in the CDC Malignant Cancer Conditions value set |
CDC malignant cancer conditions |
Condition and
Encounter
|
Condition.category, Condition.code, and Encounter.diagnosis |
Content
The following artifacts formalize the description of the logic and behavior defined by this
recommendation.
Example Data/Requests
| Description |
CDS Hooks Request |
Expected Response |
| Patient is 18 or older. Patient has been prescribed 72 HR Fentanyl 0.075
MG/HR Transdermal System (RXNorm 197696) one patch per day for 30 days. This will
trigger the message "High risk for opioid overdose - taper now" It will then link to the
"MME Conversation Tables"
"https://www.cdc.gov/drugoverdose/pdf/calculating_total_daily_dose-a.pdf" |
Request
JSON
|
Response
JSON
|
| Patient is 18 or older. Patient has been prescribed Morphine Sulfate 10
MG (RXNorm 892495) one tablet per day for 30 days. The patient will be excluded and no
message will be triggered - an empty set of cards will be returned. |
Request
JSON
|
Response
JSON
|